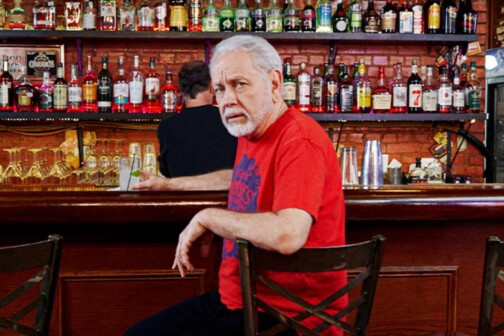
Parkland Health and Hospital System continues its quest for a new CEO, narrowing the field to four candidates earlier this month. They include current executive vice president and CFO Walter (Ted) Shaw, and three out-of-state candidates. Running the show until then is Bob Smith, interim CEO, who took over in September. A former vice president of Dallas-based Tenet Healthcare Corp., Smith came out of retirement to lead Parkland through the end of December, or until a permanent CEO is found. He talked with D Healthcare Daily about the changes that are under way at Parkland, and what lies ahead.
Q: Why did you take on the job of interim CEO?
Well, I was contacted by the board chairman and asked If I would consider the possibility of being the interim CEO. I have a long career in the healthcare industry. I’ve run hospitals and have been responsible for hospitals. And what I mean by that is I’ve had regional positions and I’ve also been the CEO of a hospital that’s a publicly traded company. So I’ve been in and around the hospital business literally all my career.
And having lived in the Dallas area off and on for 20 years I was familiar with Parkland, a number of people who worked here and or trained here as physicians, and I knew the reputation and the importance the hospital played in the healthcare industry and in the community at large. So it was an intriguing possibility to have the opportunity to have even a brief association with the hospital. I retired from a full-time career in healthcare administration at the end of December 2011. This was an opportunity for me to fulfill my desires to be a part of the healthcare industry, but not do that on a full-time, ongoing basis.
Q: What happens at the end of your contract?
I told the board that I would be here four months at a minimum while they’re doing their leadership search. We came up with an initial agreement from September 1 to December 31. I have also informed the board that if the leadership transition is not completed at that time I’ll certainly, at their desire, stay on longer, if that’s what they want and what’s necessary.
Q: So retirement didn’t suit you?
Well, I actually tried retirement once before, about 10 years ago, so I knew what I was getting into when I retired again, and I knew also that I wouldn’t be fully retired for the foreseeable future. I’ve been staying involved in professional organizations and also entertaining the possibility of interim roles. This really has been a perfect situation for someone who is at this stage in their career like I am.
Q: What changes have you implemented at Parkland so far?
There were a number of changes that were already underway organizationally, as well as improvements to the overall process of hospital management, and so we’ve continued those. When it comes to running hospitals, I don’t know if anything is ever complete. It’s an ongoing continuum of how things occur. What I’ve tried to do is bring a little bit more structure and discipline to the organization. The process had begun with others who are in the executive leadership ranks, and we’ve continued the process while I’ve been here, and I think we’re starting to see some outcomes.
Q: You mention more structure, but what does that mean specifically?
This is a very large organization. We have more than 10,000 employees, about 9,000 of them full time. So it’s an exceptionally busy organization. We see over 1 million patients a year, and that brings a lot of volume and a lot of activity to the Parkland campus. … I’ve tried to bring a little more focus and structure to the pacing of running the organization, in the context of how active the hospital is.
Q: How are you getting employees involved?
We have focus groups working at all levels of the operation in process improvement. Hospitals by their nature have to be learning organizations, because there’s always new technology and procedures, new competencies that have to be learned and developed. We have real strong focus on performance improvement, and that brings groups of varying people together—technicians, nurses, physicians, support staff to focus on a continuous learning and performance improvement process. We definitely have that going on here, just for the basic quality and patient safety care that we provide.
And then anytime we do something that’s facility related, which would be construction programs, building something new, we bring together all the groups that will be utilizing the space into the equation. (Parkland currently is developing a $1.3 billion hospital, scheduled for completion in 2014.) In the new hospital, it’s really a broad effort, as we have to plan every space of a 2-million-square-foot building. We’re increasing the size of the existing Parkland facility by 75 percent. There’s a strong collaborative effort to try to reach out to various utilizers of people who will be occupying and using the space to help plan it.
We’re bringing together nurses, doctors, support staff, and walking them through the virtual aspect of what the new hospital is going to be as they plan. We’re doing that now on a technologically enhanced basis. It’s the first time I’ve ever seen that in my career. Usually when you plan something you throw the plans on the table and everybody sits around and looks at the blueprints. This is a more virtual opportunity. It’s using, which is what the building will also use, the latest technology for us to be able to provide an ideal environment in which to care for our patients.
Q: How would you rate your experiences here so far?
I like to think it’s going well, and I believe it has. I’ve had quite a bit of exposure to our management staff. I spend as much time out and around the hospital as I can, while also attending the daily duties of a CEO. For example I spent about an hour-and-a-half today in our urgent care center in our urology clinic down in our emergency room, and in our psychiatric emergency room, being updated on what’s happening in construction, and what’s happening with improvements in care, safety, and quality. I’m trying to get out and be seen, and in a large organization that can be difficult.
I’ve been quite pleased and impressed with the quality of management and employees that we have here, as well as the loyalty and dedication to the Parkland mission. It really is something that doesn’t take long to be converted to. That transition was easy for me. But when you’re new in an organization, people have to see that and understand it and know it means something to you, too.
Q: How is your role at Parkland similar to and different from experiences you’ve had in the past?
Healthcare, generally is a calling, and in many respects, a lifestyle. It’s a business that never closes. Hospitals are always open. In that resect, Parkland is the same as all other hospitals. What happens at the bedside, the way nurses deliver care, the way doctors provide their services, technicians, clinicians—that’s really the same in every hospital, whether it’s a for-profit or not-for-profit or public facility. Day in and day out they’re the same.
What’s different about Parkland, obviously, is that it is a public hospital. Our mission is to specifically serve the underserved. And that aspect of the mission is somewhat different. It’s a broader community mission than many other hospitals have. Some hospitals serve, while they care for the patients exactly the same as we do once the patients are there, their focus is really on a very small, defined community more closely around their campus, while ours is a much broader community. And it’s not just the hospital that we have. We have 13 community-oriented primary care centers and 11 school-based clinics. We have four mobile-health vans. We provide 100 percent of the care at the Dallas County Jail.
At the end point, in terms of the individual receiving care, it’s done exactly the same. But from a focus in mission perspective, those aspects are different in Parkland than they are from many other hospitals.
Q: How would you describe your management style?
I’m known for having a situational management style. In my last position, I had about 20 hospital CEOs report to me. That meant I had to have 20 different management styles. I try to fit what I think the needs are of the executives that I work with, as those executives have different backgrounds, different experiences, and personalities. My management style is really situational, whether dealing with a hospital that has financial trouble or a hospital that has service-related problems or dealing with a hospital that has quality or safety issues, and in dealing with a management staff that are all unique individuals. I try to employ a management style that I think will be effective for whatever type of situation it’s going to be.
Q: What are your goals and plans for the remainder of the time that you’ll be at Parkland?
We are starting some new initiatives with regard to structure. The employee rank, specifically the mid-management level, is responding well and indicating that they like a little more structure, so we’re definitely going to continue that.
The other thing we’re working on is looking at driving the organization a little more from a metrics basis, developing a balanced score card that would allow management as well as the board of directors to make sure that they see—on a minimum of a monthly basis, some on a daily or weekly basis—key operating metrics that need to be responded to in running the organization. People outside of healthcare use scorecards as well. The scorecards that we’re developing have metrics in quality, safety, and metrics for employees, such as recruitment and retention, employee engagement, employee satisfaction. It also has service metrics—patient satisfaction and physician satisfaction. We’ll also be looking at the financial side, this business, the cost of operation by what our supplies cost and our personnel cost, and things of that nature.
We’re developing a metrically driven business environment, more so than what previously existed. It’s definitely something that we’re working on that’s more focused since I’ve arrived. And it’s something that the board of directors and upper management staff will be using going forward.