Since 2010, Texas has led the nation in rural hospital closures. There have been 26 hospital closures in that time period, reducing access to healthcare for rural communities and shutting down one of the area’s largest employers.
When rural families have babies who end up in the neonatal intensive care unit, that often means they make the trek to large urban centers to receive the care they need, bypassing the regional medical centers. The move takes a family away from their home and support system while the local hospital bleeds another patient. If the stay in the NICU is extended for weeks, parents who live in rural communities may have to quit their jobs or job hours a dat in order to care for and be with their newborn. It is emotionally and financially costly for the families and health system as a whole.
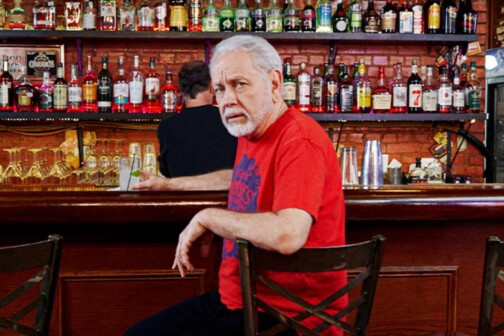
But not every hospital is willing to go quietly into the night. “Those that are surviving and continue to provide local access to healthcare are the ones who are wiling to stretch and innovate,” says John Henderson, CEO of the Texas Organization of Rural and Community Hospitals.
An innovative partnership between Children’s Health and rural hospitals throughout Texas is keeping patients at home and delivering expertise to rural providers to keep hospitals in business and patients close to home via their virtual care program.
The program has been aided by legislation. In 2017, HB 1697 created $5 million worth of resources to create pediatric telehealth resource program that would award grants to connect rural facilities with pediatric specialists via telemedicine. The grants can be used to purchase equipment or upgrade technology services to facilitate the delivery of the telemedicine.
One of Children’s Health’s first telehealth partnerships was with Childress Regional Medical Center in West Texas, where Henderson was the CEO at the time. The hospital was one of the largest employers in the area, but it was difficult to keep specialists onsite. Many were driving at least 100 miles from Lubbock to see patients in Childress.
After discussions between Henderson and Children’s Health, they decided to go ahead and provide NICU services via telemedicine. Unlike traditional medicine, most of the contact between Children’s Health and their rural partners are physician to physician consults, meaning Children’s Health docs are not becoming the physician of record, but instead providing guidance and confidence to the local physicians so that they can properly treat the newborn.
“It reassures the family that they know what they are doing,” says Tamara Perry, the Senior Director of Virtual Health Operations and Innovation at Children’s Health. “Our role is to strengthen their community hospital. What we would like to do is keep them in their community hospital.”
With Texas leading the nation in uninsured individuals and medical costs rising, costs are on the minds of all parties involved in the care of intensely ill children. Many low income rural children are on Medicaid, which means the state picks up the tab for costly care. But because of the Children’s Health consults, 53 percent of patients have been able to remain in their local hospital, for a savings of $114,000 per transport. The program has resulted in 197 teleNICU consultations since 2013, and 167 teleER consults since 2015.
The virtual consults have expanded beyond NICU care to advanced pediatric emergency care, pediatric orthopedics, and even pastoral care for those who need it. Looking forward, they hope to add fetal medicine and genetics in the telehealth program. Because of the number and diversity of cases seen by physicians at Children’s Health, they often have the experience to diagnose the unusual cases. Perry remembers one situation where a boy in Childress developed a skin rash, and local emergency physicians diagnosed it as an allergic reaction to a swimming pool. But the Children’s Health physicians had seen the reaction before, and knew it was a reaction to a staph infection that displayed through the skin.
Children’s Health does an analysis of where patients are being transferred from in order to decide which hospitals to partner with for its telehealth services, which are quite affordable for outlying facilities. The arrangement began as $3,000 per month but is now just $700 per year to have consultations available at a local medical center. Grants from the legislation have allowed the hospitals to purchase the $16,000 to $24,000 telemedicine cart, which is equipped with electronic medical record access and HIPAA compliant technology.
Perry says that she appreciates the relationships that are built between the providers, and rural physicians build confidence because they are told they are doing the right thing. “Our role is to give a hand out and up for those local rural hospitals,” Perry says.