Sarah pauses and then begins to cry. “It was terrible, those treatments. It was like totally losing control. The treatment was worse than the disease.” It is difficult, even now, for Sarah Phelps (not her real name) to discuss what happened to her after she suffered a nervous breakdown in 1971. She was hospitalized, and on 24 separate occasions, she was given what the doctors called “therapy.” She considered it torture. She was taken to a small room where electrodes were attached to her temples. Then for a few agonizing seconds, an electric current was transmitted through her brain. Now Sarah, a Dallas woman in her 40s who is a law student in Houston, has vivid memories of those moments in the room where the shocks were administered. “I’d kill myself,” she says, “before I’d let anyone give me shock treatment again.” Electroshock treatment, invented in Italy in 1938, has been hailed as a cure for a wide number of otherwise intractable psychiatric disorders. It has also been condemned as little more than torture by some of the patients who have been forced to undergo the shocks, and even by some psychiatrists and clinical psychologists. The treatment is not without supporters, including some former patient
“Shock treatment helped me,” says Roland Sanchez (not his real name), who was hospitalized in Dallas in the early Seventies suffering from a depression that was wrecking his marriage and his career. “There are some things I still don’t remember from before I was hospitalized, but mostly it’s come back. I’m really grateful to my psychiatrist. Everything’s different now. I’m a lot stronger.”
The treatment that Roland praises and Sarah damns is called by a number of different names, including electroconvulsive therapy, shock treatment, EST, electrotherapy or, most commonly, ECT. For many years after its introduction, it was used as a cure-all, but by the mid-Seventies it had been supplanted in most places by new types of psychotropic (mind-affecting) drugs and newly developed psychotherapies. Scientific tests of ECT’s actual usefulness were done, and little by little the broad spectrum of “indications” for which ECT was prescribed shrank: Even its most vigorous proponents no longer claimed the treatment was advisable except in emergencies and for a specific type of severe depression. It appeared to many that ECT was going the way of medical fads such as bloodletting, thalidomide and phrenology.
But recent developments – including the recognition that drug treatment is not the panacea for psychiatric problems that was hoped for and often carries the risk of dangerous side effects -have sparked a resurgence in the use of ECT in Dallas and throughout the state. Doug Cameron hopes to short-circuit that resurgence.
“I don’t want to have ECT made illegal, but I think it has been abused, and like any powerful tool it needs to be controlled,” says Cameron. A playwright and mental patients’ rights activist living in Austin, Cameron was involuntarily committed to Terrell State Hospital, east of Dallas, in 1973. There he was given a series of ECT treatments against his will.
“There were 70 to 100 people being forced to take shock treatments every other day, just on my ward,” Cameron says. “I’ve seen estimates that there were thousands of people being shocked in the state hospital system each year. It wasn’t treatment, it was control -the best way they could think of to handle an overcrowded population. Psychiatrists seem to have a hard time understanding this, but it was dehumanizing to stand in a long line in the hospital three times a week, scared half to death, waiting your turn to go into the shock treatment room.”
Released from Terrell State Hospital in the fall of 1973, Cameron went through more turbulent times. Slowly his life became calmer, but he didn’t lose his sense of outrage when he thought of being forced to receive electroshock therapy. Last year he joined in a 5-year-old federal suit against the State of Texas Department of Mental Health and Mental Retardation (TMHMR), which administers the state’s public mental hospitals.
“When the case started in 1975, there was what amounted to a federal investigation into state hospitals, and a new set of rules went into effect systemwide which really cut down on the amount of shock being given,” says Cameron. “The new rules required ’informed consent’ -that is, an explanation of the benefits and risks involved, and a specific consent by the patient before treatment could begin.”
In cases of a medical emergency in which no consent could be obtained, Cameron says, another psychiatrist had to give a supporting opinion, and objective proof of the emergency was required.
“The use of ECT in the system dropped dramatically,” Cameron says. “In 1980 supposedly only 30 people in the whole TMHMR system were given ECT.”
The case, titled R.A.J, v. Kavanaugh, was settled last year. Under the settlement, a three-member panel is appointed to oversee a series of agreed-upon changes in the TMHMR syste
To Doug Cameron, the most important part of the settlement is the stipulation that TMHMR policies on ECT cannot be changed without the approval of the panel members. This means, he says, that TMHMR efforts to liberalize the rules on ECT are effectively blocked, at least for now. One such attempt was made earlier this year, when the department proposed changing ECT from a “treatment of last resort” to a “treatment of choice” for a number of conditions.
“Psychiatrists say they need the option for certain emergency cases,” Cameron says. “This may be so. But the record is clear that ECT has been consistently abused, and we need legal controls so that such abuse is prevented. People should be able to consent to ECT, after being fully informed of its possible side effects. But if they don’t consent, some other form of treatment should be used.”
Juanita Kirby, M.D., a psychiatrist in private practice in Dallas, says, “For some patients ECT is actually the safest, most effective form of therapy we can give. It can save lives. Admittedly there has been overuse and even abuse- for example, using ECT as a punishment. Theoretically, if a doctor did that, you could file a lawsuit for malpractice. But when you get the legal system involved in telling doctors what they can do, it doesn’t help anyone. A medically proven treatment should be available anytime. And the reason for getting a second opinion is that you don’t trust the first one.”
Not all psychiatrists agree. Dan Creson, M.D., of Galveston, who acted in behalf of the plaintiffs when R.A.J, v. Kav-anaugh was first filed, says, “Although ECT is well accepted as beneficial in suicidal depressions, it is easy to overuse it. I have to be concerned about physical interventions like ECT, which have psychosocial implications which are not always recognized. For example, when you give someone a pill, that pill carries a lot of messages besides just the chemical message-it includes messages about how you are to think about yourself and your relationships with other people. This is also true of drastic interventions such as ECT.” Creson says the effect can be harmful rather than curative -reinforcing a patient’s view of himself as dependent and out of control.
Private hospitals in Texas have changed their use of ECT. According to Juanita Kirby, psychiatrists at Timberlawn, where she served her residency, used ECT regularly while she was in training there. However, Doyle Carson, a psychiatrist now at Timberlawn, says that to his knowledge ECT was administered to only two patients last year. Other private hospitals around the state have reported a decline in numbers of ECT treatments, but statistics. show that ECT is still used more often in private than in publicly operated facilities.
The multiplicity of opinion expressed by psychiatrists about ECT is not unique to this one subject. And that brings up an important point: A person who wants help with a psychological problem and who randomly picks a name out of the Yellow Pages really has no idea what he is going to come up with. There is a bewildering array of treatments and strategies and practitioners-strict Freudian analysts, psychotherapists from any of a dozen conflicting schools, religious and gay counselors, and believers in the somatic, or physical, causes and cures of mental illness.
The major point of struggle about ECT and other intrusive physical interventions – such as drugs and psychosurgery – is what is referred to as “the model” of mental function, or more specifically, the model of mental illness.
The “medical” model holds that mental illness is an event that takes place in the brain of the individual – an electrochemical imbalance that causes aberrant behavior and can only be treated by someone with a medical school degree, using whatever components of the “armamentarium” that are necessary.
The “humanistic” or “dynamic” model regards mental illness as a far less concrete entity -as symptoms or behavior that arise out of conflict between people or between parts of the mind. The users of this model tend to see problem situations, rather than aberrant individuals. The only therapeutic intervention that makes sense in this model is working out the conflict.
The interplay between these two models and the tensions over the use of ECT are best seen by examining an institution that dominated the history of scientific psychiatry in Texas until very recently. That institution is the University of Texas Medical Branch (UTMB) Department of Neurology and Psychiatry. In 1970 it was estimated that more than half the psychiatrists in the state had trained at UTMB, and even more had gone to medical school there for at least part of their training. UTMB-trained psychiatrists treat thousands of patients in Houston, Galveston, Dallas, Austin- even in towns as small as Buda. Since 1970, other psychiatric residence programs have developed, and practitioners have moved into the state, diluting UTMB’s influence, but it is still considerable.
UTMB’s psychiatry department developed an unsavory reputation along the way. People still joke that Houston Lighting and Power must own UTMB because ECT is used there so frequently.
That reputation bears examining, even though it is largely untrue: The implication is that all the psychiatrists at UTMB are “shock docs,” and that the treatment has been discarded elsewhere. Psychiatrists at Parkland Memorial and Presbyterian Hospitals in Dallas use ECT, and the technique is still taught at Baylor Medical School in Houston, where students refer to it as “jump starting.” Many psychiatrists trained at UTMB never use ECT. Nevertheless, the UTMB psychiatry department has become identified with ECT and other somatic treatments for mental illness, and that identification has a historical basis.
To a remarkable extent the construction of the model for psychiatry in Texas and throughout the Southwest was the work of one man, Titus Holliday Harris. Born in Fulshear, west of Houston, in 1892, Harris attended the Allen Academy and Southwestern University in Georgetown, near Austin. There he received a B.A. degree and distinguished himself, he later told an interviewer, mostly with his athletic ability. He chose to enter medical school rather than become a professional athlete because his Methodist family didn’t approve of playing sports on Sunday.
Harris received an M.D. degree from UTMB in 1919, interned at the adjacent John Sealy Hospital in 1920 and joined the university’s faculty in 1920, specializing first in internal medicine and later in neurology. In 1926 he was appointed head of the newly created Department of Neurology and Psychiatry.
When Harris first set up his department, psychiatry was one of the lowest-paid and least-popular specializations. But, under Harris’ leadership, the faculty grew, eventually attracting more residents than any other special residency program at UTMB. Under Harris, it was also an innovative program administratively: “Anticipating a current by 40 years, it was also the first to embrace the concept that psychiatric patients are most successfully treated in a general hospital setting,” according to an official UTMB history.
In 1947, Harris and three of his former students became partners in the new Titus Harris Clinic, housed in a building on the UTMB grounds, paid for by the Sealy-Smith philanthropic foundation. Set up to handle the burgeoning flow of private patients, it was by all reports a very lucrative practice – and it became very important to the medical school as a source of patients.
According to Dr. Edward Gripon, a UTMB-trained psychiatrist now on the staff of UTMB and a member of the Titus Harris Clinic, “Galveston as a community couldn’t support more than three or four psychiatrists, and there are almost 30. That’s because it is a major referral center for the entire state.” To this day patients referred to Galveston are important to the medical center, and in the early days of the psychiatry department, Gripon says, “going to Galveston was synonymous with going to the mental hospital.”
Harris is described by former colleagues as an inimitably curious man, one with a forceful personality, who set his personal stamp on the department he created, and through his students, on psychiatrists all over the Southwest. He remained head of the department until 1962 and continued in private practice until his death in 1969. That year an association of UTMB-trained psychiatrists was formed. Named the Titus Harris Society, it first had about 20 members. The membership grew to more than 200, with many members in influential academic and administrative posts.
Under Titus Harris, shock therapies – particularly ECT -were installed as the major interventions for treating mental illness.
Francis Braceland, an East Coast psychiatrist who was a contemporary of Harris’, provides an explanation for the ready acceptance of these therapies in a paper he published in 1969. Psychiatrists, he said, were then suffering from a furor therapeuticus – an irresistible urge to do something, however drastic, to alleviate the suffering of their patients. “It should be remembered,” he wrote, “that in the 1930s, young men did not rush into psychiatry in great numbers. Those who did were jeered at by their colleagues, who warned them that the illness was catching.”
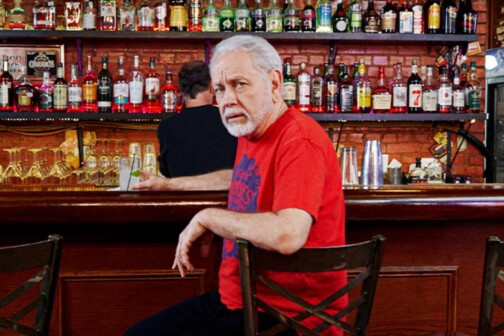
Martin Towler, 71, a native of Hockley, Texas, was a medical resident when he administered the first ECT treatment given at UTMB. A board-certified neurologist as well as a psychiatrist, renowned for his research in the development of electroencephalography, Towler is a short, heavy-set man with gray hair, a florid complexion and a husky voice. Towler says he administered that first ECT in 1937 or 1938 to one of faculty member Hamilton Ford’s patients, a young woman in her mid-20s suffering from depression.
“I’ve never forgotten the patient I gave that first treatment to,” says Towler. “Of course, our technique was different then. We didn’t put the patient to sleep. We tried to use the minimum current, and ended up giving the young lady a sub-minimum amount, not enough to cause a convulsion. She had only a fleeting period of fuzziness. When the next day we increased the amount of electricity and found the right amount, we noticed a dramatic improvement in the patient.”
“This young lady was suffering from depression,” he says. “It’s a disease with classical symptoms, the same in everybody regardless of race, creed or color, like malaria or a kidney stone. In the overwhelming majority of cases of depression and schizophrenia, the disease is neurobio-chemogenic. It’s certainly not psychogenic.” The clinical success of ECT shows over and over the validity of this model, Towler maintain.
At first treatments were administered in what is now called “classic ECT” style: anywhere from 90 to 140 volts of electricity delivered through two metal electrodes placed bilaterally over the patient’s temples, lasting for a period of anywhere from .2 seconds to almost 10 times that long. During the treatment, the patient underwent what looked like a grand mal epileptic seizure (in fact the first shock therapy was introduced by a Hungarian physician who made the mistaken assumption that epileptics could not have schizophrenia), with a general disruption of brain functions and a violent two-phase physical convulsion. Broken bones caused by the convulsions were an occasional complication at this time. The patient would often experience amnesia, confusion, nausea, headaches and fea
An important advance was made at UTMB about a year and a half later, Towler says: He and his colleagues were among the first in the country to introduce the use of paralyzing agents and anesthesia along with ECT – by preventing the muscular manifestations of the seizure, these cut down the number of fractures during ECT, and the anesthesia spared the patient the unpleasant choking sensation brought on when both the ECT and the muscle-paralyzing drug immobilized his diaphragm. Many physicians argued against the use of the modifications with ECT, Towler says.
The safety of the ECT procedure they developed at UTMB, Towler points out, compares favorably with that of a number of other surgical procedure
Edward Gripon says that the period that followed saw the extension of ECT to every problem that came to the psychiatrist’s attention, not only at UTMB but worldwide. “ECT was overutilized everywhere. But you have to remember that the urge was to find a way to help, and there wasn’t much else that worked for some conditions. It was like penicillin, which was found useful for some things, then was overprescribed and has now fallen into disfavor. There was shock therapy, some narcotics -that and prayercloths. So ECT was used in some clinical situations where we know now it is of no help at all.”
The use of ECT spread, and hospital populations grew rapidly during this period, as did the department. By the mid-Sixties, the full-time department staff had grown to 32 (it currently stands at 45), and the number of beds had climbed to almost 300 (now reduced to 75). At its peak, the department was training 18 residents each year (now reduced to 10 per year).
Figures for most of the late-Sixties are not available, according to department chairman Robert Rose, but a survey of a two-month period in 1966 shows that 212 treatments were given, almost 1,300 per year. That number has decreased to an average of less than 60 per two-month survey period, he says, or about 400 per year.
The number of ECT treatments given at UTMB began to decline in the late-Sixties because of a number of factors. The most important was the development of a new generation of antipsychotic and antidepressant drugs, which made it possible for the first time to stop “warehousing” people with long-term mental problems and to treat them in their own communities. The packed, understaffed and increasingly expensive public mental institutions around the nation began to show their first population declines after decades of steady increases.
But another factor also played a part, according to current and former staff members: The department grew faster than it could train people to fill slots in its faculty. Faculty members came to the psychiatry department from outside UTMB, bringing with them, in many cases, a much more psychological, as opposed to somatic, orientation. Eugene McDanald and Robert White, both psychoanalysts, joined the staff, as did a number of psychologists and social workers.
A real split from UTMB’s orthodox medical model was made when a team of researchers, including three psychiatrists, two psychologists and a social worker, directed by psychologist Harold Goolish-ian and psychiatrist Eugene McDanald (who later became a member of the Titus Harris Clinic) developed a new type of brief, intensive psychotherapy for families with disturbed adolescents called multiple impact therapy. This work became the foundation for continuing investigation into the dynamic model of mental illness not just in Galveston but nationally.
Goolishian says that at first the “family therapy” movement, as it came to be called, had little influence in the psychiatry department. “We were trying to broaden the mandate of psychiatry to include input from the behavioral and social sciences,” he says. “But we were regarded as a fringe group and given very little in terms of resources or access to students.” The “mainstream” of the department continued using the same methods it had developed during the Forties and Fifties.
“We were trying to work out family therapy as a clinical practice and made considerable progress, but along with that we developed it as a theoretical position,” Goolishian asserts. “It is a way of viewing the kinds of problems we refer to as symptoms, arising from the struggle within and between people and systems, attempts to resolve the issues raised by life itself. Family therapy changes the focus of treatment from the individual to the individual functioning within a system, such as, for example, a family. As a theoretical position, it’s a direct challenge to the medical model of mainstream psychopathological psychiatry, which aims to describe the disease within the person, assuming that you can understand the person outside the social context.”
In 1970 the ferment within the department culminated in the creation of the new Division of Community and Social Psychiatry, headed by Goolishian and Dan Creson, M.D., a psychiatrist who had taken his residency at UTMB and then gone back to school, earning a Ph.D. in anthropology from Rice University. For the first time practitioners of the dynamic model had real access to students and department resources, Goolishian and Creson say.
Other members of the faculty remained uninfluenced by these new therapies, as shown by the case of former mental patient Tony Powell (not his real name) and his treating psychiatrist, Dr. Winston Martin, UTMB graduate, faculty member and Titus Harris Clinic member.
“Winston Martin made even his colleagues at the Titus Harris Clinic seem timid,” says one of his former colleagues, now practicing in another city. “He thought of himself as a man on the frontier, stamping out symptoms to keep civilization from being overwhelmed.”
Tony Powell, a native of Norman, Oklahoma, who had attended high school in Fort Worth, made A’s through four years at the University of Texas at Arlington, and joined the Delta Theta fraternity there, entered UTMB’s medical school in 1969. Popular, outgoing and athletic, he was happily married and he was elected president of his class. He did above average work for his first three years in Galveston. A dispute with one of his professors-a psychiatrist -ended, however, with Tony being required to take all his third-year classes over. Tony, with no other choice, acquiesced, but became angry and frustrated.
What happened next is unclear: Tony says he was persecuted by a conspiracy of powerful people; others say Tony got involved with illegal drugs and had a psychotic breakdown. Tony says he went to the office of the professor with whom he had had the earlier dispute, intending to confront him. The professor, Tony says, refused to talk to him
The following morning, two police officers came to Tony’s house, he says, struck him, knocking him to the ground, handcuffed him and dragged him to their car. Tony was kept in solitary confinement for a week at the county jail, where he was observed by another psychiatrist. The anger and fear Tony plainly showed were noted in his evaluation, later filed with the court, and were ascribed not to Tony’s incarceration but to his illness. His wife refused to sign a commitment authorization. Tony says that after a hearing conducted at night in the locked mental ward of one of the UTMB hospitals (for which he had neither preparation nor legal representation), he was declared mentally ill and committed for 90 days. There he was placed under the care of Winston Martin.
Tony has been unable to obtain his records, either from the hospital or from Martin’s files. What he has is a Social Security Administration memorandum okaying payment for some of the treatment he received in 1972, when the “over-utilization” of ECT and other shock treatments was commonly supposed to have been a thing of the pas
Eight years later Tony is trying to pick up the pieces of his life. He is living on a farm in Oklahoma, gardening, writing a book.
“I don’t have words to express how I feel about the people who did that to me,” he says. “One of the worst things is they had my own classmates administering the shocks to me -that’s how I found out that I had received not only the 187 shocks listed in that memorandum, but also a number of [other] treatments which didn’t find their way into my records.”
The use of such large numbers of shock treatments to treat schizophrenia is part of what has been called by various proponents intensive shock therapy, blitz electric shock therapy, depatterning treatments and regressive electroconvulsive therapy
According to a study published in Diseases of the Nervous System in 1951. patients given regressive ECT “showed profound disturbances. They were dazed, out of contact and, for the most part, helpless. All showed incontinence of urine, and incontinence of feces was not uncommon. Most of them were underactive and did not talk spontaneously. Many failed to respond to questions but a few patients would obey simple requests. They appeared prostrated and apathetic. At the same time most of them whined, whimpered and cried readily, and some were resistive and petulant, in a childish way. They could usually be made to walk if led and supported, but their movements were slow, uncertain and clumsy. Most of them liked to be coddled. Masturbation was not uncommon. They seemed to have lost all desire to eat or drink and showed no discrimination as to what they were eating. They had to be spoon-fed, and most of them lost from 3 to 12 pounds in weight during the course of treatment. They could not dress themselves; and none of those tested during this period could complete the task of extracting a match from a matchbox and lighting the match.”
Former colleagues of Winston Martin say he used intensive ECT often, believing strongly in its potency as a treatment. Unfortunately, Martin is not available to comment on Tony’s case: He disappeared under mysterious circumstances on the night of December 24, 1976
Sergeant Bob Steen, spokesman for the Galveston Police Department, says a missing persons file on Martin is still kept open.
It has been suggested that he went to a bar on the night of his disappearance, perhaps became intoxicated and was picked up by someone who then robbed and killed him. Steen adds: “That is a possibility, but it is also a possibility that he is digging ditches in Idaho or something, under a new identity because he wants it that way
The retirement of Titus Harris’s successor, Hamilton Ford, in 1975, followed by Martin’s disappearance, coincided with a number of other changes in the department. A review committee for psychosurgery and experimental procedures was set up by Harold Goolishian and others -regressive ECT, insulin shock and other treatments were declared experimental.
An annual inspection by the national Joint Commission on the Accreditation of Hospitals issued a report severely criticizing the psychiatry department’s physical plant and threatening to withdraw accreditation unless new facilities were constructed. Then a new chairman was appointed from outside the department. Robert Rose brought with him a formidable academic reputation and firm convictions about the way the department should be run. He quickly began reshuffling the organization
“There was a brouhaha when I became chairman,” he says. “Before, the Titus Harris Clinic was not very separate from the administration of the department. Now it’s different. Members of the clinic still teach here and have admitting privileges. But the administration of the department is different.”
Whereas ECT has been abused in the past, Rose says, it is still a valuable tool in a limited number of areas. “Exaggerated claims both for and against ECT are wrong. It should not be used except in suicidal depression or violent mania, when other methods have been given a chance to work, but have failed. Then it can be lifesaving.”
Currently, ECT is used in about 4 percent of the cases treated at UTMB, Rose says: Twelve out of the 15 patients in a recent survey treated with ECT had physicians from the Titus Harris Clinic attending them. Most important, he says, is the limitation now in effect on the number of ECT treatments-14 -that can be given in one course.
Coincidentally, with the change in the rules under Rose at UTMB, a number of psychiatrists from the Harris Clinic began to admit their patients in the newly built psychiatric facilities of St. Mary’s Hospital, a private facility across the street from UTMB.
At the same time that some UTMB psychiatry graduates are referring patients back to members of the Titus Harris Clinic for ECT, other UTMB-trained psychiatrists are involved in a pro-ECT group devoted to promoting the treatment within the profession and in the public consciousness-and lately, even in the White House.
This organization, the International Psychiatric Association for the Advancement of Electrotherapy (members are plumping for the use of “electrotherapy” to replace other terms, because, they say, “the worst thing about the treatment is the name,” which scares people off) is a kind of gold-key club for ECT specialists-it costs $100 to join and the annual dues have just been raised from $50 to $75. The group was formed in 1975 to counteract the effects of legislation and court actions restricting ECT, as well as to improve the reputation of the treatment in the public estimation.
During the last session of the Texas Legislature, a bill restricting the use of ECT in Texas was sponsored by Rep. Sam Hudson of Dallas and State Sen. Chet Brooks of Houston. Currently, psychiatrists in state-operated institutions can administer ECT to their patients only if they obtain “informed consent.” Failing that, they must have the concurrence of two other psychiatrists to the treatment. These are regulations within the state system, but they are not law.
The bill, written by Doug Cameron, would have legally defined informed consent, changed the state’s current rules to law and extended the provisions of the law to private institutions as well. It was at first opposed by hospital and medical industry lobbyists, who argued that the law was unnecessary, as private hospitals already abided by a voluntary standard of informed consent. After part of the bill was modified, however, these industry lobbyists withdrew their opposition. The measure passed the House and was voted out of committee in the State Senate, but failed to gain final approval before the end of the legislative session.
Losing ground scientifically, legally and professionally to more modern and more progressive therapeutic strategies, the proponents of ECT -now led by a UTMB-trained psychiatrist, who taught students there for 10 years -are being driven to political activism.
It remains to be seen whether this viewpoint will again be established as the ruling orthodoxy in Texas: If so, Terrell Hospital may again be giving ECT to hundreds of patients daily.
Get our weekly recap
Brings new meaning to the phrase Sunday Funday. No spam, ever.
Related Articles
Local News
In a Friday Shakeup, 97.1 The Freak Changes Formats and Fires Radio Legend Mike Rhyner
Two reports indicate the demise of The Freak and it's free-flow talk format, and one of its most legendary voices confirmed he had been fired Friday.

Local News
Habitat For Humanity’s New CEO Is a Big Reason Why the Bond Included Housing Dollars
Ashley Brundage is leaving her longtime post at United Way to try and build more houses in more places. Let's hear how she's thinking about her new job.
By Matt Goodman

Sports News
Greg Bibb Pulls Back the Curtain on Dallas Wings Relocation From Arlington to Dallas
The Wings are set to receive $19 million in incentives over the next 15 years; additionally, Bibb expects the team to earn at least $1.5 million in additional ticket revenue per season thanks to the relocation.
By Ben Swanger