The rumors were strongest the Tuesday after this past Memorial Day. Staffers had seen well-dressed investors prowling the administrative floor of Dallas’ shiny Walnut Hill Medical Center, ducking into conference rooms to huddle with executives. Buyout rumors, then talk of outright closing had been in the air as the hospital’s inventory of on-hand medical supplies dwindled. Patient volume had suddenly cratered, both in elective procedures and in the emergency department. As a result, the “official” demise of the independent, physician-invested hospital on June 2 was almost anticlimactic. There was a single sheet of wide-ruled-lined paper with the words “ER Closed” crudely scribbled on it, plus another note taped to the facility’s front door telling patients to go to a nearby competitor.
The $100 million, 100-bed, for-profit Walnut Hill hospital opened in 2014 in the face of adversity. Consolidation in the healthcare industry had been swallowing up independent operators, creating megamergers under systems that could better manage a huge patient population through data. The mergers gave the hospitals more leverage when determining rates with insurance providers. Carriers were increasingly shifting away from reimbursing based on volume and toward proven value, fueled partly by new federal healthcare regulations.
According to a 2017 survey by the American Hospital Association, just 12 percent of the nation’s 5,564 hospitals—689—are not part of a system or in some kind of network. The AHA defines a system as a “multihospital organization or a diversified single hospital system,” and a network as “a group of hospitals, physicians or other providers working together.” Within North Texas, the Dallas-Fort Worth Hospital Council estimates there are 25 independent, physician-owned entities in this market—out of 122 overall, according to U.S. News & World Report.
Walnut Hill, in many ways, was among the last of its kind in Dallas: a luxurious, standalone facility that tried to punch above its weight at big guns like Baylor Scott & White Health and Texas Health Resources. Housed in a renovated, eight-story, 1980s-era building at the corner of Greenville Avenue and Walnut Hill Lane, it practically thumbed its nose at its catty-corner neighbor, Texas Health Presbyterian Hospital Dallas. Its business model allowed it to do what similar, physician-owned competitors couldn’t because of federal law: accept Medicare and Medicaid patients. Walnut Hill’s closest competitor, the similarly upscale Forest Park Medical Center chain, which was physician-owned, failed last year after exorbitant out-of-network fees dried up; the final nail for Forest Park was an alleged fraud scheme by some of its founders.
Walnut Hill, which was funded by investments from doctors and with operating capital from the sale of its real estate to a Florida-based investment trust, hoped it could survive and thrive on high-quality patient care, cutting-edge medical technology, a variety of specialty services, and luxurious add-ons like a chef-driven restaurant and a movie theater. Its plan was to lure caregivers by providing a work environment that fostered a “family-like” culture, one where doctors had a voice in how the hospital was run and what equipment was purchased. But “The Nut,” as the hospital was affectionately called by doctors, nurses, and staffers, wouldn’t make it past year three.
In contrast to system-owned hospitals, which have the money and patient volume to cover their costs, standalone Walnut Hill could neither afford its extravagant expenses nor attract the patients it needed to keep its doors open. “Managed care rates and growing competition make it so they can’t thrive anymore,” Cory Countryman, who was the hospital’s CEO, said of independent facilities like Walnut Hill. “There’s so much consolidation these days with hospital systems, [with] the economies of scale to make [the systems] work.”
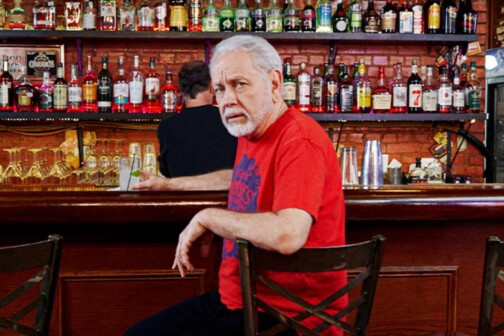
Countryman was an executive who’d spent time at hospitals in Weatherford and the small southeast Texas town of Cleveland before being approached about the top job at a new hospital in Dallas. He says he was intrigued by the ambition, sold on “a dream hospital that was physician-involved, bringing high-quality and high-acuity care. You never get an opportunity to do a standalone hospital with a model like that,” he says. “The model and culture were extremely attractive to me.”
The founders enlisted the healthcare architecture firm Page Southerland Page to query patients and then to build something that would accommodate their desires. The building on Walnut Hill was gutted from the inside and rebuilt to upscale standards. Visitors got free valet parking. Expensive art was hung on the walls throughout the open-floor layout. Patients luxuriated in beds with 300-thread-count sheets. Tall windows facing north afforded beautiful views of foliage near the Royal Oaks Country Club and Harry Moss Park. There were hotel-quality cafeteria meals and an in-house Starbucks. A Forbes magazine contributor called Walnut Hill “The Hospital Steve Jobs Would Have Built.”
The hospital also spared no expense with its service lines. It offered cardiology, diagnostic imaging, gastrointestinal services, orthopedics, rehabilitation, an emergency department, and a cardiovascular operating room for emergency open-heart surgery. There were dozens of private suites, even in the typically open intensive care unit. The hybrid ORs boasted the technology to stream what was happening into teaching hospitals. Countryman once bragged that Walnut Hill had received more than 7,000 applications from practitioners, making it “tougher to get into [than] Harvard University.”
Walnut Hill’s physician-invested model allowed it to treat patients on Medicare and Medicaid after receiving approval from the Joint Commission, which certifies hospitals. This expanded the number of patients the facility could potentially attract. While federal law barred physician-owned facilities (like Forest Park) from treating publicly insured patients, Walnut Hill’s model was different. In a 2014 article in D CEO Healthcare, the hospital’s Lyle Rountree explained: “The federal Stark law does not allow Medicare and Medicaid beneficiaries to get care at a hospital from a physician who has a financial relationship with that entity. The physicians behind Walnut Hill created a construction corporation that paid for the building. They do not receive payments on a sliding scale based on volume or type of care. … They are lenders to the operating company, which is separate, and they receive the same amount of money each month.”
Walnut Hill was owned by Nashville-based Surgical Development Partners, a healthcare service provider, and Houston-based Medistar Corp., a real estate development firm for medical facilities. Florida’s Carter Validus Mission Critical REIT pumped more than $99 million into buying it and served as the hospital’s landlord. By the time Walnut Hill closed in June, however, Chapter 7 bankruptcy filings showed it owing between $100 million and $200 million to 650 different creditors. Meantime, revenue had been just $10 million to $50 million annually.
Unfortunately for Walnut Hill, there would be no sale to a larger system—no buyout from some investor waiting in the wings. In August, all its assets were auctioned to pay off its obligations.
To get Walnut Hill off the ground, Countryman says he was charged with bringing an administrative team on-board and establishing the hospital’s procedures and policies from scratch. He also was tasked with obtaining the necessary licenses and safety credentials and with creating regulations. That process took six to eight months. Throughout the startup period, however, the hospital was burning through an undisclosed amount of cash.
“Every day that you’re open, doing dry runs and what’s necessary, you’re paying money to employees, paying money for trials,” Countryman says. “We opened up underfunded. It’s a startup, and those are hard. Especially when you’re not part of a system.” In contrast, hospitals that open under corporate systems typically have regulations and the necessary protocols already in place.
Walnut Hill opened “underfunded,” Countryman contends, because it was overbuilt. The first day it opened for patients, it was fully furnished and operational. That’s unusual, experts say, because most facilities open with just a few floors furnished to care for the expected volume of patients. As the number of patients increases, the hospital can expand as necessary to meet the demand.
Walnut Hill’s administration set a goal to break even by year three. But two months after its third anniversary, it became clear that there was “no more financial opportunity,” according to bankruptcy documents. Just before Memorial Day weekend, Capital One Bank, the hospital’s primary lender, decided it would no longer fund the facility, and the hospital lost its operating capital. Countryman spent the long weekend meeting with investor groups that had expressed interest in buying Walnut Hill. “We had four business days to make a deal happen, or we had to close,” he recalls. “But you just can’t come up with that money in a short amount of time to make a deal.”
The hospital’s board members declined to comment for this story.
The Tuesday after the long holiday weekend, Countryman received word that the hospital would have to close the following Friday. The employees were paid, and the staff refocused its efforts to having patients discharged or transferred to other hospitals. “We wanted to make sure everyone was taken care of before we closed the doors,” Countryman says.
Even now, some patients and staffers speak highly of the failed experiment. Former patient Lorraine Rooney, 45, says she’s heartbroken that she won’t be able to return to Walnut Hill for care. “I went there two times between February and April 2017, because I was having asthma attacks,” she says. “I went there because it had such high reviews. I went back again because they took care of me so well and had my records.”
Former staffers say there were telltale signs of trouble, though. Alex Gnaedig, a Walnut Hill trauma nurse who worked closely with the ER department head, recalls the visits from the investors, and reports having had to work with dwindling supplies. Two months before the hospital closed, Gnaedig remembers, surprisingly few patients were coming through the ER. “On average, we were seeing five patients a night,” he says. “But depending on the size and staff of a hospital, [you should be seeing] at least 100 [patients] per day. We weren’t hitting those numbers.”
When Gnaedig and other staffers finally got word of the hospital’s fate, they were surprised to learn the news only a couple of days before the closure. “Just give people some notice,” Gnaedig says with irritation. “A few days before does not work.”
When Walnut Hill finally locked its doors in early June, a note taped to the right-hand corner of its entryway doors read: “If you have a medical emergency please call 911 or go to the nearest hospital, which is THR-Presbyterian …” In late September the note was still affixed to the door, and the hospital’s driveway signs remained shrouded in silver tape.
Meantime, Countryman was asked whether he had any regrets—or if, in retrospect, he would have done anything differently. “The people, the concept, all of that was incredible,” the former CEO replied after a long pause. “Initially, we got out of the gate. But we never got out of the financial hole.”
The $100 million, 100-bed, for-profit Walnut Hill hospital opened in 2014 in the face of adversity. Consolidation in the healthcare industry had been swallowing up independent operators, creating megamergers under systems that could better manage a huge patient population through data. The mergers gave the hospitals more leverage when determining rates with insurance providers. Carriers were increasingly shifting away from reimbursing based on volume and toward proven value, fueled partly by new federal healthcare regulations.
According to a 2017 survey by the American Hospital Association, just 12 percent of the nation’s 5,564 hospitals—689—are not part of a system or in some kind of network. The AHA defines a system as a “multihospital organization or a diversified single hospital system,” and a network as “a group of hospitals, physicians or other providers working together.” Within North Texas, the Dallas-Fort Worth Hospital Council estimates there are 25 independent, physician-owned entities in this market—out of 122 overall, according to U.S. News & World Report.
“We got out of the gate. But we never got out of the financial hole.”
Cory Countryman, CEO of Walnut Hill
Walnut Hill, in many ways, was among the last of its kind in Dallas: a luxurious, standalone facility that tried to punch above its weight at big guns like Baylor Scott & White Health and Texas Health Resources. Housed in a renovated, eight-story, 1980s-era building at the corner of Greenville Avenue and Walnut Hill Lane, it practically thumbed its nose at its catty-corner neighbor, Texas Health Presbyterian Hospital Dallas. Its business model allowed it to do what similar, physician-owned competitors couldn’t because of federal law: accept Medicare and Medicaid patients. Walnut Hill’s closest competitor, the similarly upscale Forest Park Medical Center chain, which was physician-owned, failed last year after exorbitant out-of-network fees dried up; the final nail for Forest Park was an alleged fraud scheme by some of its founders.
Walnut Hill, which was funded by investments from doctors and with operating capital from the sale of its real estate to a Florida-based investment trust, hoped it could survive and thrive on high-quality patient care, cutting-edge medical technology, a variety of specialty services, and luxurious add-ons like a chef-driven restaurant and a movie theater. Its plan was to lure caregivers by providing a work environment that fostered a “family-like” culture, one where doctors had a voice in how the hospital was run and what equipment was purchased. But “The Nut,” as the hospital was affectionately called by doctors, nurses, and staffers, wouldn’t make it past year three.
In contrast to system-owned hospitals, which have the money and patient volume to cover their costs, standalone Walnut Hill could neither afford its extravagant expenses nor attract the patients it needed to keep its doors open. “Managed care rates and growing competition make it so they can’t thrive anymore,” Cory Countryman, who was the hospital’s CEO, said of independent facilities like Walnut Hill. “There’s so much consolidation these days with hospital systems, [with] the economies of scale to make [the systems] work.”
Fine Sheets, Beautiful Views
Countryman was an executive who’d spent time at hospitals in Weatherford and the small southeast Texas town of Cleveland before being approached about the top job at a new hospital in Dallas. He says he was intrigued by the ambition, sold on “a dream hospital that was physician-involved, bringing high-quality and high-acuity care. You never get an opportunity to do a standalone hospital with a model like that,” he says. “The model and culture were extremely attractive to me.”
The founders enlisted the healthcare architecture firm Page Southerland Page to query patients and then to build something that would accommodate their desires. The building on Walnut Hill was gutted from the inside and rebuilt to upscale standards. Visitors got free valet parking. Expensive art was hung on the walls throughout the open-floor layout. Patients luxuriated in beds with 300-thread-count sheets. Tall windows facing north afforded beautiful views of foliage near the Royal Oaks Country Club and Harry Moss Park. There were hotel-quality cafeteria meals and an in-house Starbucks. A Forbes magazine contributor called Walnut Hill “The Hospital Steve Jobs Would Have Built.”
The hospital also spared no expense with its service lines. It offered cardiology, diagnostic imaging, gastrointestinal services, orthopedics, rehabilitation, an emergency department, and a cardiovascular operating room for emergency open-heart surgery. There were dozens of private suites, even in the typically open intensive care unit. The hybrid ORs boasted the technology to stream what was happening into teaching hospitals. Countryman once bragged that Walnut Hill had received more than 7,000 applications from practitioners, making it “tougher to get into [than] Harvard University.”
Walnut Hill’s physician-invested model allowed it to treat patients on Medicare and Medicaid after receiving approval from the Joint Commission, which certifies hospitals. This expanded the number of patients the facility could potentially attract. While federal law barred physician-owned facilities (like Forest Park) from treating publicly insured patients, Walnut Hill’s model was different. In a 2014 article in D CEO Healthcare, the hospital’s Lyle Rountree explained: “The federal Stark law does not allow Medicare and Medicaid beneficiaries to get care at a hospital from a physician who has a financial relationship with that entity. The physicians behind Walnut Hill created a construction corporation that paid for the building. They do not receive payments on a sliding scale based on volume or type of care. … They are lenders to the operating company, which is separate, and they receive the same amount of money each month.”
Walnut Hill was owned by Nashville-based Surgical Development Partners, a healthcare service provider, and Houston-based Medistar Corp., a real estate development firm for medical facilities. Florida’s Carter Validus Mission Critical REIT pumped more than $99 million into buying it and served as the hospital’s landlord. By the time Walnut Hill closed in June, however, Chapter 7 bankruptcy filings showed it owing between $100 million and $200 million to 650 different creditors. Meantime, revenue had been just $10 million to $50 million annually.
Unfortunately for Walnut Hill, there would be no sale to a larger system—no buyout from some investor waiting in the wings. In August, all its assets were auctioned to pay off its obligations.
What Went Wrong?
To get Walnut Hill off the ground, Countryman says he was charged with bringing an administrative team on-board and establishing the hospital’s procedures and policies from scratch. He also was tasked with obtaining the necessary licenses and safety credentials and with creating regulations. That process took six to eight months. Throughout the startup period, however, the hospital was burning through an undisclosed amount of cash.
“Every day that you’re open, doing dry runs and what’s necessary, you’re paying money to employees, paying money for trials,” Countryman says. “We opened up underfunded. It’s a startup, and those are hard. Especially when you’re not part of a system.” In contrast, hospitals that open under corporate systems typically have regulations and the necessary protocols already in place.
“We had four business days to make a deal happen, or we had to close,” Countryman recalls.
Walnut Hill opened “underfunded,” Countryman contends, because it was overbuilt. The first day it opened for patients, it was fully furnished and operational. That’s unusual, experts say, because most facilities open with just a few floors furnished to care for the expected volume of patients. As the number of patients increases, the hospital can expand as necessary to meet the demand.
Walnut Hill’s administration set a goal to break even by year three. But two months after its third anniversary, it became clear that there was “no more financial opportunity,” according to bankruptcy documents. Just before Memorial Day weekend, Capital One Bank, the hospital’s primary lender, decided it would no longer fund the facility, and the hospital lost its operating capital. Countryman spent the long weekend meeting with investor groups that had expressed interest in buying Walnut Hill. “We had four business days to make a deal happen, or we had to close,” he recalls. “But you just can’t come up with that money in a short amount of time to make a deal.”
The hospital’s board members declined to comment for this story.
The Tuesday after the long holiday weekend, Countryman received word that the hospital would have to close the following Friday. The employees were paid, and the staff refocused its efforts to having patients discharged or transferred to other hospitals. “We wanted to make sure everyone was taken care of before we closed the doors,” Countryman says.
A Caring Staff
Even now, some patients and staffers speak highly of the failed experiment. Former patient Lorraine Rooney, 45, says she’s heartbroken that she won’t be able to return to Walnut Hill for care. “I went there two times between February and April 2017, because I was having asthma attacks,” she says. “I went there because it had such high reviews. I went back again because they took care of me so well and had my records.”
Former staffers say there were telltale signs of trouble, though. Alex Gnaedig, a Walnut Hill trauma nurse who worked closely with the ER department head, recalls the visits from the investors, and reports having had to work with dwindling supplies. Two months before the hospital closed, Gnaedig remembers, surprisingly few patients were coming through the ER. “On average, we were seeing five patients a night,” he says. “But depending on the size and staff of a hospital, [you should be seeing] at least 100 [patients] per day. We weren’t hitting those numbers.”
When Gnaedig and other staffers finally got word of the hospital’s fate, they were surprised to learn the news only a couple of days before the closure. “Just give people some notice,” Gnaedig says with irritation. “A few days before does not work.”
When Walnut Hill finally locked its doors in early June, a note taped to the right-hand corner of its entryway doors read: “If you have a medical emergency please call 911 or go to the nearest hospital, which is THR-Presbyterian …” In late September the note was still affixed to the door, and the hospital’s driveway signs remained shrouded in silver tape.
Meantime, Countryman was asked whether he had any regrets—or if, in retrospect, he would have done anything differently. “The people, the concept, all of that was incredible,” the former CEO replied after a long pause. “Initially, we got out of the gate. But we never got out of the financial hole.”