The National Committee for Quality Assurance (NCQA) last week launched a patient-centered specialty-practice (PCSP) recognition program.
The panel will recognize specialty practices that meet standards for care coordination and information-sharing between specialty and primary-care providers. Specialists must show they use a systematic approach to tracking patients and include them in management of their care. Delivery and payment systems also must meet NCQA requirements.
NCQA is considered the gold-standard recognition for patient-centered medical homes (PCMH) for primary care practices. There are 26,000 primary-care providers at 5,500 NCQA-accredited medical home sites
Although all specialties and subspecialties are eligible for the program, the PCSP is especially suited for oncology, endocrinology and cardiology, according to Patricia Barrett, NCQA’s vice president of product development.
Specialty practices will be measured by six standards, including tracking and coordinating referrals and patient care; patient communication and access; planning and managing individual patients and patient populations, and showing improvement over time.
Margaret O’Kane, NCQA’s president, said in a webinar that 57 early adopters have already signed on to the program. She predicted that payers would use the recognition program to steer referrals and potentially to create care-coordination payment opportunities for specialists.
O’Kane outlined the case for specialty care coordination:
- The typical primary-care physician coordinates with 229 physicians in 117 practices annually.
- The average Medicare beneficiary sees seven physicians and fills more than 20 prescriptions a year.
- The average elderly patient has two referrals a year.
- Specialist visits comprise more than half of outpatient physician visits.
- Disconnected communication goes both ways. Primary-care physicians say they send patient information for referrals 70 percent of the time while specialists report receiving it only 35 percent of the time.
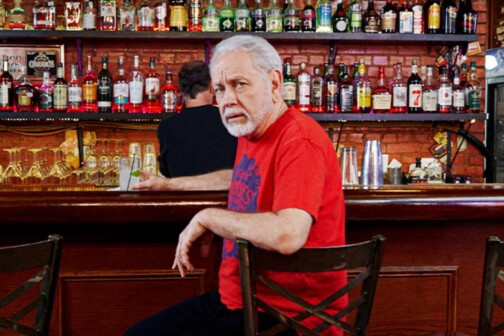
Dallas oncologist John Cox, MD, was one of the PCSP framers and early adopters of the program. His Texas Oncology practice is composed of 10 oncologists and two radiology oncologists at two Methodist Health System hospitals. He also has outreach offices in Corsicana, Waxahachie and Ennis.
Cox, who is also editor-in-chief of the Journal of Oncology Practice, represented the American Society of Clinical Oncology in developing a 2010 American College of Physicians white paper called The Patient-Centered Medical Home Neighbor.
Cox estimates that his practice has more than 500 referring physicians, and is somehow touched by more than 1000 physicians annually. He said the NCQA effort is to establish the role of specialty practices in relation to PCMHs and to give structure to how they organize their referral networks. The central issue, he said, is care transitions.
“Everything should be centered around patient needs. In the past 20 to 40 years, we have created a strong system of providing care based on fee-for-service. We have a wonderful distribution of services. But they are all siloed, and more hard siloed than ever. Science has become more complex, with more multispecialty involvement. We are very good at providing cancer care under our roof. We are not as good at navigating different silos of care,” he said.
Cox noted that specialists perform a substantial amount of primary care.
“Many patients rely on us to be their primary medical home. Most primary-care doctors don’t want anything to do with complex cancer cases. In some cases, the roles are going to be reversed. I may refer the patients to a primary-care doctor to get their high blood pressure under control,” he said.
Cox said the NCQA specialist program is the “first comprehensive yardstick” he has encountered that will guide him in improving his practice. He said the practice is reviewing electronic health record effectiveness, and talking to other practices about how to share information more efficiently.
“One of the more exciting things we are doing is referral agreements. They have nothing to do with money. It’s all about the process of how we get them and how we communicate back. Practices are pretty excited about this. Doctors have been very frustrated (about the lack of communication),” he said.
Steve Jacob is editor of D Healthcare Daily and author of the new book Health Care in 2020: Where Uncertain Reform, Bad Habits, Too Few Doctors and Skyrocketing Costs Are Taking Us. He can be reached at [email protected].