When I was 3 years old, I was diagnosed with Type 1 diabetes. The chronic disease has never been a big deal for me. It’s obnoxious, sure, but manageable. Over the course of my 34 years, I estimate I’ve given myself some 55,000 injections. I’ve worked hard to stay healthy. I have run a few half-marathons and completed a full. I’m not a fast runner, and I never particularly enjoyed it, but I knew my diabetes would catch up to me at some point, so I ran because I could.
About three and a half years ago, everything changed. I was part of a group of women called Leadership Texas. It was a yearlong program with which we traveled to different cities and learned about the people making a difference. One of our sessions was in Amarillo. The second day of the trip, on a Saturday, I woke up in my hotel room soaked in sweat. Every part of my body was swollen. I couldn’t bend my fingers, my toes, my elbows, or my knees. I was exhausted beyond description.
I had joined a study a year and a half prior to see if a medicine that is used on Type 2 diabetics could work for Type 1s. It had been a great 18 months, with lower blood sugars and weight loss. But then I changed jobs and, thus, insurance companies. The new company didn’t like the name-brand drug. They made me switch to a generic.
That morning in Amarillo, I figured I was having a reaction to this new drug. I was convinced that things would go back to normal in a few weeks. I was certain it was just a small bump in the road.
I was wrong.
What follows are my Facebook posts over the years, lightly edited, as I saw nearly a dozen doctors in an effort to figure out what was wrong with me.

June 23, 2016
For the past six weeks, my entire body has been swollen. My joints have hurt so much that I haven’t been able to do simple things like walk down stairs or make a fist. I’ve had nightly fevers, daily low-grade fevers, and extreme fatigue. A couple nights ago, my rheumatologist called me with an urgency in her voice. She had reviewed my labs, and she was extremely concerned about my liver (she even mentioned liver failure). She told me I had to cancel next week’s trip to Toronto, and she said she was considering putting me in the hospital. I asked for options. She said that if I saw her friend, a dermatologist, in the morning, and got a biopsy of the rash on my leg, we could figure out next steps.
So this morning I went to see the dermatologist, and I think (I hope, I pray) we figured out what’s wrong with me: I have drug rash with eosinophilia and systemic symptoms (DRESS) syndrome. Basically, it’s a rare syndrome that’s a result of a horrible reaction to a drug.
Thank you to the doctors who finally gave me a diagnosis; everyone who has heard me complain and offered help; and to my husband, David, for being my hands, arms, and knees these past few weeks. A diagnosis is just the beginning, but at least I now know where to start.
One fun thing: because of me, a company has to add a new side effect to its medicine bottle.
July 22, 2016
I’m beyond thankful to Carolyn from Dallas and the three women from Paris who came to my rescue this afternoon. Apparently, liver failure + a 100-degree day + a one-hour walk around downtown parks = me nearly passing out across the street from my apartment. Those four women are my angels.
August 6, 2016
It’s been about six weeks since we figured out that I have DRESS syndrome. I’ve been joking that I had liver failure. And, while I’m still on a lot of steroids (#roidrage is a thing, my friends), my liver numbers are better, and things have settled down. I have been told it’ll be January before I get everything back to normal. Essentially, this whole thing will affect me for 10 months.
It all started with a letter from my insurance company saying it wouldn’t cover my medicine and wanted me to switch.
I just got another letter. My insurance company doesn’t want to cover my brand of insulin. It wants me to switch that, too.
I called. I wanted someone/anyone there to know what his/her decisions have done to me. I got the most amazing woman on the line, who just so happens to be a Type 1 diabetic who has taken some of the same medications I have. She was wonderful. While I’m not sure my complaints will go anywhere, it at least helped to know that there are actual human beings at the insurance company who not only understand but are also going through the same things.
March 27, 2017
There’s a special place in pill hell for any medicine that causes fatigue and insomnia.

August 23, 2017
Over the past few months, I have thrown myself into work and various city engagements. I thought that at some point, the DRESS syndrome would end/be cured/whatever the appropriate term is. I got off the steroids, which prompted every single symptom to return, worse than before. My rheumatologist finally posed the question of whether DRESS syndrome is actually what I’m dealing with.
I consider the past few months my dark months. Every morning, when my alarm goes off, the first thought is “Do I have the strength to put my feet on the ground?” My hands are so weak that I can’t turn the knobs on my shower or twist the lid off my shampoo bottle. My legs are so weak that I can’t sit on a chair. My ankles are so swollen that I can’t wrap the straps of my sandals around them.
Everything hurts.
I’ve seen endocrinologists, rheumatologists, dermatologists, allergists/immunologists, and gastroenterologists. If one more of them tells me I’m fine, I may lose it. If I hear, “This isn’t my wheelhouse, you need to see someone else,” without a recommendation for who that someone else is, I may lose it.
Sadly, reading between the lines of what my doctors are saying, I think they’re telling me I already have lost it.
November 27, 2017
This one’s long. My apologies.
A couple months ago, I was put in touch with a woman who has similar symptoms to mine: weak muscles, extreme fatigue, chills/fevers, mysterious rash. Whatever is wrong with her is way worse than what I have going on. But we did bond over the fact that all we want out of life is to be able to put our bras on without any help (it’s the little things). Talking to someone who shared the same frustrations was therapeutic in so many ways. She told me about her doctor and said I should check out his office. She also mentioned her treatment: a small dose of chemo in the form of methotrexate.
The next day, David and I went to the movies and saw The Big Sick. Based on a true story, the movie focuses on a woman who has something called Still’s disease. I looked it up after. I swear it’s what I have. I went down a rabbit hole and started reading blogs by one doctor who focuses on Still’s. Come to find out: that doctor is in Dallas, in the same office as the doctor of the woman I talked to the day before.
“I get to work in a field that truly makes a difference with people who are beyond passionate in cities that are tackling challenges.”
I immediately made an appointment. For reasons out of my control, I was unable to see him until today. I took a folder that has about 40 lab reports in it; photos; and a document with a timeline, symptoms, and doctors and their recommendations. I showed him everything I had. He asked me questions but didn’t say much else. Then he walked over to look at my fingers, which were purple, scaly, and clubbed. “Oh, Lordy,” he said.
He left and came back with a light and his assistant. The assistant looked at my nails using the light while the doctor explained to me that they were seeing “wormlike” movements in my cuticles. The assistant’s response? “Cool.” The doctor said that patients don’t normally like their conditions to be considered “cool.”
“I don’t mind, just as long as you have a diagnosis,” I told him.
He gave me one. He said it’s scleroderma, an autoimmune disease. I’m not convinced it’s scleroderma, but I do believe the autoimmune part, which basically means my body is attacking healthy cells it sees as foreign bodies. We’re going to do all the labs. It’s rare. Basically, fewer than 300,000 people have it. (I’m special!) There are two versions of it, too. One’s OK. The other, which involves the lungs, isn’t so great. The doc is pretty sure I have the good one. Labs will confirm if he’s right.
If it seems weird that I’m putting this all out there, it is. This whole thing is weird. The human body is weird. I’ve been given two diagnoses over the past two years. Both times, the doc says what I have, hands me a printout (one was from Wikipedia), asks if I have any questions (oh, do I?), and then sends me on my way. Then I’m left to process. To determine if it’s accurate. To imagine my new life. To write weird Facebook posts.
This isn’t the worst diagnosis I could’ve received. (It’s a chronic disease, but I’ll live, somewhat comfortably with treatment.) It’s not the best. (Over time, it’ll stretch my skin and could cause a lot of issues around the mouth/throat and my abilities to swallow.) It’s just what it is. I’ll run some labs, take my meds, and one day, hopefully, I’ll be able to put my bra on by myself, because, dammit, it’s the little things.
November 28, 2017
David has been my rock these past few months. Yesterday, when I got my diagnosis, I called him and said I didn’t think I’d ever be normal again. “I won’t be able to get dressed on my own,” I whined.
“Well,” he said. “That’s why I’m here.”
February 7, 2018
I started my day at the doctor’s office, where I was told it’s time to up the amount of chemo I’m taking. (Don’t worry: it’s a tiny, tiny amount in pill form for autoimmune issues.) Also, I got a surprise bill and an order for a slew of new (expensive) tests.
Then I went to the office, where our team of 10 from Akron and Dallas was building our first digitally fabricated mobility parklet. At the Better Block, we’re constantly working to find ways to give communities the tools they need to reshape the built environment. Through a parklet, we can take a space set aside for the car and use it for people. I can’t wait to share what we’re working on.
Then I sat in a circle with some of Dallas’ brightest minds, discussing social equity in urbanism as part of Greater Dallas Planning Council’s urban design task force. Then I had my first Dallas Center for Architecture board meeting, where I met the team for the programming partnerships task force.
I told a friend the other day that, medically, I’m a mess. But me? I’m OK. In fact, I’m pretty freaking #blessed.
I get to work in a field that truly makes a difference with people who are beyond passionate in cities that are tackling challenges. It doesn’t always work out. But there’s always tomorrow. And while I have tomorrow, I have another chance to make the world better.
March 3, 2018
Today I had a work appointment at Medical City. While I waited for my ride outside the ER, I overheard a woman tell a nurse that she didn’t really know the woman she was waiting for.
“I was her Uber driver for her first dialysis appointment,” she said. “When she told me she didn’t have anyone to take her, I told her that from then on, I’d take her.”
So she does.
May we all be more like her.

March 28, 2018
The other day, I talked to Leadership Dallas about my health conditions as part of health day. The group, which is made up of leaders around the city, had spent the day hearing from the experts at hospitals, insurance companies, and nonprofit orgs. They wanted my perspective as a patient.
It was a rambling mess of me trying to explain exactly what was happening (which is hard to do when you don’t actually know what is happening). At the end, someone in the audience raised her hand and said, “I am so pissed for you. Just so angry. Can you tell us where you were failed? Who can we point a finger at?”
“Well, the first thing that has failed me is my body,” I told her. I’ve always attempted to do right by it, but at the end of the day, having Type 1 diabetes since I was 3 has worn it down. A car wreck as a young adult took its toll. And now my body is literally attacking itself. If we’re starting somewhere, let’s start there, I told her.
Then we can go to the insurance companies, Big Pharma, Congress, and doctors.
Yes. Many doctors failed me. I was ignored. I was told everything was fine. I was given a misdiagnosis. When I complained about my hands, I was told I need to stop washing them so much. When I complained about my mysterious weight loss, I was congratulated. I was told by the very first specialist, a rheumatologist, that my disease wasn’t in her wheelhouse.
A year and a half and nearly 10 specialists later, I was back in her office (though not to see her) and told I had autoimmune diseases. If that’s not her wheelhouse, I don’t know what is.
I explained to the group that I had started researching medicine and women, and I was shocked to find that the way medicine in women is approached is abysmal. Several studies have found that research is primarily done on male subjects, which means that women could get the wrong dosages. And many of our symptoms are dismissed. A 2011 study found that animals in medical research are up to five times more likely to be male than female. Tests, cures, doses—they are all set up for men, not women.
So, where was I failed? Everywhere. And I’m not alone.
April 13, 2018
One of these days, I won’t have a health update. Today’s not the day.
I’ve had a change in diagnosis. Here’s where I am: Type 1 diabetes. We already knew about this one.
Raynaud’s. It causes the vessels in my fingers to narrow and makes it hard for blood to get to them. Whenever I’m even slightly cold, my fingers turn white and blue. This is the reason you’ll see me wearing gloves in the grocery store this summer.
Interstitial lung disease. Pretty annoyed about this. Basically, there is scarring in my lungs, which causes them to stiffen. This is what’s making it difficult for me to catch my breath and is causing me to cough obnoxiously.
Dermatomyositis. This replaces scleroderma. The doc made a change to the diagnosis because he saw the rash on my knuckles (honestly, I hadn’t even realized it was a rash). I asked the doc if this was good news, worse news, same news. He said, “You don’t want either of them. But I’m cautiously optimistic.” Optimistic because, unlike scleroderma, DM has more than a 10-year life expectancy. Cautious because it is super connected to cancer. But it appears cancer chances are really high in the first year and go down after. I’m in year three. But I have to do more tests to rule various cancers out.
So, not much changes with the diagnosis. It’s still a rare autoimmune disease that affects my skin and joints. But now, because of the lung disease, I have to stop taking chemo. So on to a new drug, a new diagnosis (or two), a new threat, and some new hope.
April 17, 2018
When it comes to my healthcare, I have all the privilege in the world. For now, I have the money I need to take care of my health the way I see fit. I have options for transportation to get to my appointments. I have a job that’s flexible to allow me to get to my appointments. I have a life flexible enough to allow me to navigate insurance’s murky waters. I have a laptop that I can use in the waiting rooms so I can work remotely. I have time because I don’t have to worry about taking care of someone who’s dependent on me.
And, yet, I’m exhausted.
I do not know how I could physically continue if I didn’t have just one of the above privileges. But I know that is the reality for a majority of Americans.
April 21, 2018
One of the country’s biggest Earth Day festivals happens every year in Fair Park. As part of the Better Block, we’re activating the empty plaza in front of The Hall of State. I’ve also partnered with a friend to interview some of the attendees. Over the past 24 hours, I have interviewed 25 people and one owl. I have talked to some of the most incredible people about what they’re doing to make our world better.
But the discussion that will forever stick with me: the one I had yesterday with a volunteer. Somehow, we started talking about health. Through the course of the conversation, she told me she was diagnosed with dermatomyositis when she was 33.
“HOLY S***!” I said. “I was diagnosed with that literally a week ago!”
We talked for another 45 minutes, about her symptoms, my symptoms, her treatment, my treatment. And while she talked, it suddenly hit me: she’s normal! Her hands are fine! She’s able to sit in a chair without trouble! She’s off steroids!
I can’t tell you how wonderful it was to talk to her. There are 9.63 dermatomyositis cases in every 1 million people. And the two of us were sitting in a parklet in the middle of Fair Park talking about how we both have it. This is what I love about my job. We’re all about activating spaces so complete strangers can sit together and have a conversation. We never know what could come of those little moments. But we love to think of the possibilities.
June 9, 2018
Evil.
By June 1, I had already billed $30,000 to my insurance. I have not had any big events. No hospital stays. No surgeries. That amount is merely for doctors, a few tests, and medicine. If I didn’t have insurance, I would be f*cked.
June 17, 2018
Four weeks ago, my doctor forbid me from riding a bike. Not that he really needed to. Ever since I lost muscle two years ago, I’ve been able to go only a few blocks before my legs turn to Jell-O.
As part of my work at the Better Block, however, I’ve been asked to organize and lead a group of 20 or so community leaders from the United States to a study tour of Copenhagen, exploring its bicycle infrastructure, public spaces, and processes. The only vehicle we’re using to navigate the city: bikes.
I told my doctor it was literally impossible for me to not be on a bike. He looked me straight in my eyes and said, “You have a serious disease. You need to be careful.”
Luckily, Copenhagen’s bike share program is made up of electric bikes (meaning they’re pedal assisted). Today, I rented an e-bike, and for the first time in forever, I was able to keep up, ride the entire route, and actually enjoy it. For those of us with limited mobility, e-bikes can open so many avenues (and streets and trails). They truly can be life changing.
June 24, 2018
I realize that if I share all the bad health updates, I should also share the good ones. So here’s a good update: today, for the first time in two years, I made a fist with my right hand. I’ve grown to really appreciate the little things.
August 25, 2018
What it looks like when you climb 460 steps with interstitial lung disease. Worth it to get this view of Florence.
September 8, 2018
Death. I think about it a lot. When you have a chronic disease, the idea of death is never too far from your mind. It’s not that I think my diseases will kill me tomorrow. It’s that I see the small impact they’re having over time.
But this isn’t about pity. It’s about death. And that doesn’t depress me. If you spend much time around me, you know that at some point, I’ll try to talk to you about it. It’s not that I’m trying to make you feel uncomfortable. It’s just that I think it’s something we should be comfortable discussing. I also think that recognizing death causes you to truly live.
And that’s why, when I found Claire Wineland a couple months ago, I fell in love. Claire, 21, was born with cystic fibrosis and constantly lived with death. She wrote and spoke about it, and I’ve found her take on death so refreshing, so beautiful, so hopeful. She was willing to talk about it, and she was unafraid of it.
If you have not heard this woman speak, please listen. She spoke many truths, my favorite of which is: “Death is inevitable. But living a life that we are proud of, that is something that we can actually control.”
December 30, 2018
My meds aren’t working. If you’ve been around me lately, you’ve been annoyed by my cough. Sometimes it’s just a cough. Sometimes it builds to the point of me needing to leave the room to throw up. It’s annoying, always.
I started the journey earlier this year with a small pill form of chemo. But because we discovered interstitial lung disease, I had to change to a med that transplant patients use. But now we’re talking about me doing a biological medicine through an infusion. From everything I’ve read, it works, especially with those who have lung involvement.
Unfortunately, insurance doesn’t like to cover it. So my doctor is fighting for me. But even if it is approved, there’s the question of how much will be covered.
Healthcare should be a right, not a privilege. But that’s not the way it works in this country. I know ACA isn’t perfect. But instead of constantly trying to dismantle it, we should leave what works and tweak the elements that need to be changed. And give those of us who are fighting a chance to live.
(I should also mention: compared to where I was a year ago, I’m better. I have gained back muscle. My hands still aren’t strong and, of course, the cough. But, in general, I know what’s wrong, and I have a couple options. So I truly believe I will get better.)
January 25, 2019
Today, I got my first round of Rituxan, which many have referred to as a “miracle drug.” It was an infusion that lasted six hours, and I go back in two weeks for a three-hour round. Then I should be symptom free anywhere from six months to three years. And, fingers crossed, I can finally get off steroids and lose the moon face and weight.
Before I went back to get the infusion, I read all the side effect warnings, and I imagined an IV in my arm for six hours. It was enough to make me want to turn around. I’m glad I didn’t.
There have been a lot of times throughout this three-year process when I’ve wanted to not get a test or go through a treatment. I’m terrified of needles (unless I’m in charge of them). And I’ve heard too many awful things about different tests.
“Getting your blood drawn won’t even register as pain 90 percent of the time (just tell them not to dig to avoid that 10 percent).”
But I’ve learned that things aren’t as bad as they seem. Mammograms are not a big deal. Getting your blood drawn won’t even register as pain 90 percent of the time (just tell them not to dig to avoid that 10 percent). And infusions are a great way to get some work done with free wifi and no interruptions.
The one time I completely chickened out was two months into the process. I had a rash on my leg. My doc sent me to a dermatologist to get a biopsy. The dermatologist took one look, left, and came back with a printout of a Wikipedia page explaining his diagnosis. “You don’t need a biopsy!” he said. I was so afraid of a biopsy and so elated at his news that I didn’t even question it.
I should have. It took two years to figure out what was going on. Had I gotten that biopsy, we would have known then what was wrong.
So, long post short: get the tests, research the treatments, and talk to people who have gone through them—and don’t trust a Wikipedia diagnosis.
January 31, 2019
When I was at my sickest point, I remember a vivid moment while trying to get home from work. I was standing at the bus stop across from my office. The stop is indicated with a metal pole and the bus schedule. The pole is on the edge of a grass lot. There are a lot of weeds around it.
I had lost muscle in my trunk, and lifting my foot to get up the curb onto the uneven ground was a challenge. It was a hot day, and every part of my body was inflamed. The heat caused my already swollen hands to swell more. I’m more sensitive to the sun than most, and I was taking a beating.
There was nowhere to sit. There was nowhere to hide from the sun. And I was trying to stand on uneven ground.
Finally, the bus arrived. Because I didn’t look like I needed it, the bus didn’t lower (no fault to the driver on this), and as I attempted to raise my foot and hoist myself up, I fell onto the bus.
It wasn’t my greatest moment.
But it did open my eyes. We have to have better bus stops. At the very least, people deserve a place to sit or get a bit of shelter.
February 2, 2019
That infusion I had last week? It billed my insurance $42,000. And that was just round one of two. It better work. (Thank God I have decent insurance and don’t have to pay that total!)
February 13, 2019
I lost a lot of hair in this whole being sick thing. But it’s finally back! It brought some grays with it, however. I want to embrace the grays, but I’m 34 and just not ready yet. So I decided to color my hair and get some highlights.
Halfway through the process, it suddenly hit me: I had had an infusion of Rituxan just a few days prior.
“Oh, no!” I exclaimed. “I recently had an infusion! Is that bad?”
“Naw,” said my hairdresser calmly. “I’m sure it’s fine.”
I immediately started googling, searching message boards, and trying to see if we should stop.
He calmly carried on.
After not finding anything, and seeing how relaxed he was, I put my phone away. We finally got to the point of him rinsing my hair out. He gets the first layer of foil off, and runs his hands through my hair.
Him: “Oh, thank goodness! Your hair isn’t falling out!”
Me, shocked: “Was that a real concern of yours?!”
Him: “Kinda.”
July 14, 2019
This week, I got a CT scan to check on my interstitial lung disease. During check-in, I found out my doctor changed my diagnosis to pulmonary fibrosis without telling me.
It’s awhile before I can get in to see her again and go over the results of my scans, so I do what any person with a new disease and access to the internet does: I consult Dr. Google.
And, as always, Dr. Google tells me I’m dying (in three to five years). So, yesterday, David and I booked a trip to Paris in December. Any tips for where to eat, stay, and what to do?
July 22, 2019
This morning’s call with my doctor:
Me: “Hi, there. So. It appears my diagnosis was changed from interstitial lung disease to pulmonary fibrosis. Just checking in to see what’s going on.”
Doc: “Oh, that’s not really what it is. You have ILD. It could get to pulmonary fibrosis, but we’ll just stay on it.”
Me: “Why did they say it was pulmonary fibrosis at my appointment?”
Doc: “It’s just semantics.”
Me: “Well. No. It’s not JUST semantics. With one, I have a long life outlook. With the other, I have three to five years.”
Dr.: “You’re fine.”
Me: This is the second time I’ve been told a diagnosis of a disease with a life expectancy of three to five years is “semantics.” I beg to differ.
 August 19, 2019
August 19, 2019
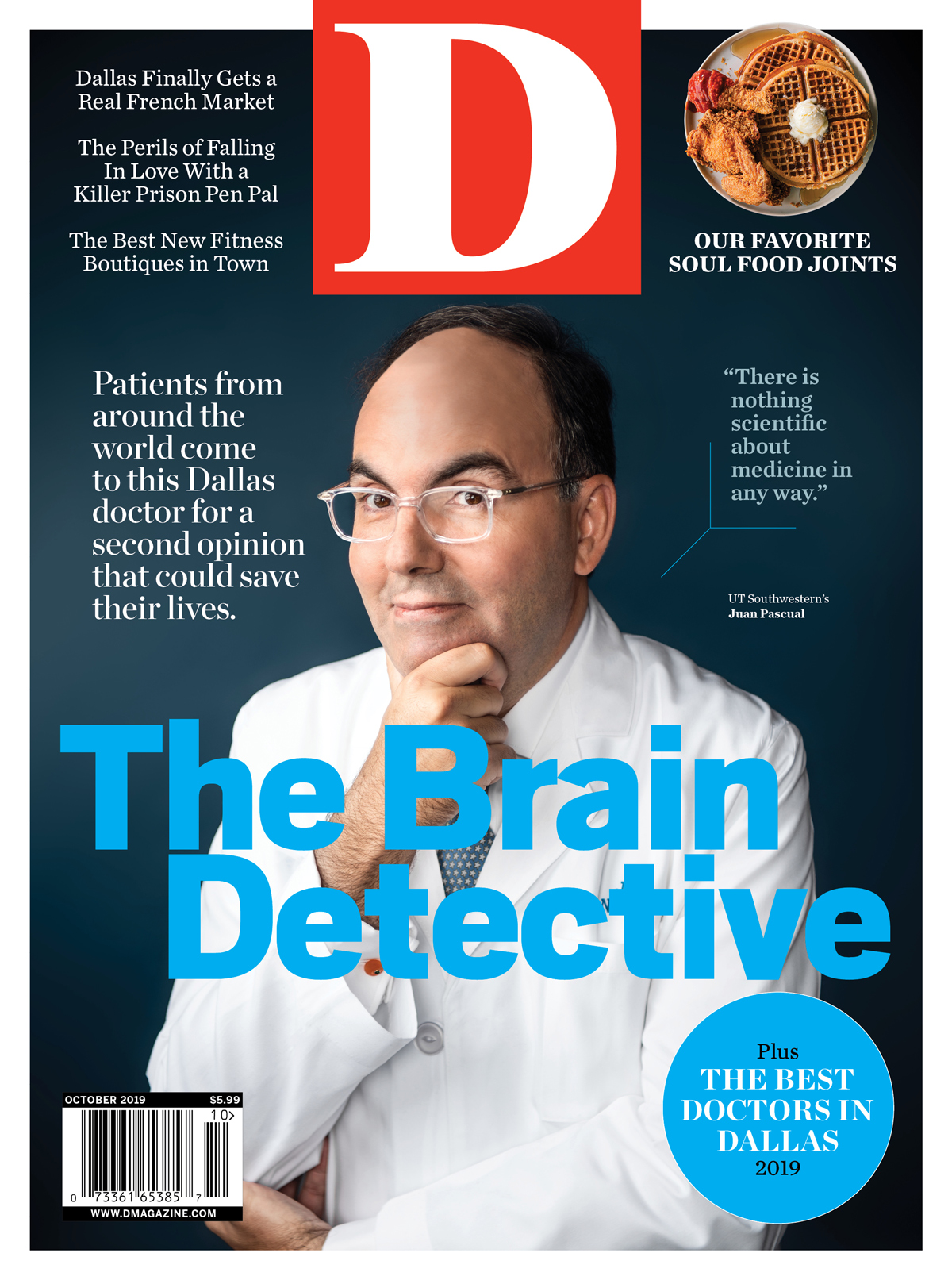
I’ve been asked to compile all my posts about my autoimmune disease journey for a health story in D Magazine, where I used to work. I have more than 5,000 words going back to 2016. I had forgotten so many of these things. (I blame this memory loss on a ridiculous amount of steroids, an autoimmune disease that’s done a lot of weird things to me over the past three years, and age.) But one of the strangest things about rereading these posts is that at my sickest point, I hardly said anything. The editor asked me why.
For one thing, I was afraid it would come across as a pity party. I was having a really hard time, which most of you knew if you saw me in person. But I didn’t think it was appropriate to share on social media. For another, I worried (and still worry) about how talking about my health could be used against me.
So, what changed? November 27, 2017, I did my first truly honest post about everything that was going on. And this was when I decided I would share more, because I realized that not only were people listening, they were living this with me. I had so many people (all women) who reached out to tell me they were going through similar things. I had so many people offer help, and even a couple said they’d gather funds to send me to a specialist they knew of.
Having lived with a chronic disease since I was 3, I didn’t think a new one would shake me. I was wrong. But I realized the difference between my diabetes and these autoimmune diseases is that with diabetes, I had a support system with several family members also having Type 1. But because my autoimmune diseases are so rare, I didn’t have that support system. It’s true that misery loves company. And because I started sharing openly about what was going on via social media, I finally found my company.