Illuminated by hot spot-lights, the object of their attention lay visible through a gaping hole deliberately cracked in his chest. Masked physicians surrounded James Kilgore,* supine and silent on an operating table at Methodist Medical Center. Kilgore’s heart lay strangely still as the red and yellow and white tissues around it were painstakingly cut and sewn.
Kilgore’s heart bypass operation, now an almost routine procedure, ended after three hours. As usual in most open-heart operations, the doctors pumped into Kilgore’s body four to six units of blood products: some combination of platelets, red blood cells, fresh frozen plasma, and cryoprecipitate, all furnished by The Blood Center at Wadley, to help stop the bleeding.
But the usual didn’t work this time. Five or six hours after the first operation, Kilgore was rolled back into the operating room while the surgeon tried to find out what was making him lose such enormous quantities of blood. Twenty units, forty units, sixty units. Still Kilgore’s blood refused to clot. His life leaked slowly away.
More than seventy units of blood later, Kilgore’s bleeding slowed, then stopped. The process took seventy-three units altogether, each given by a donor who lay down on a couch and volunteered blood to Wadley. In April 1985, several weeks after almost bleeding to death on the operating table, Kilgore went home to recover from the surgery, his rehabbed heart circulating the blood of people he would never meet.
The Gift of Life, Wadley often calls it in the center’s brochures. But this gift brought death.
Fifteen months after receiving his transfusions, Kilgore was notified in a procedure called “lookback” that one of the donors whose blood he had received had given blood again. This time, a test revealed the unthinkable. The donor had the AIDS virus. And now, further tests showed, so did Kilgore. And his wife.
On July 9, 1988, forty-three-year-old Kilgore died, as thousands have, from complications from AIDS.
But his death looks less like a lost race with medical technology and more like a random corporate killing, a case of death by negligence.
Because of this simple fact: James Kilgore received his blood on March 12, 1985-five days after Wadley uncrated the first test kits approved by the federal government to screen blood products for AIDS. The test admittedly wasn’t perfect; it actually screened for antibodies to the AIDS virus, not the virus itself. And scientists knew there was a “window” of infectivity before antibodies appeared in the blood, during which the donor might be able to transmit the disease. Still, if used properly, the test promised to prevent a large percentage of tranfusion-related AIDS cases-and might well have prevented the death of James Kilgore. Health professionals had known since January 1985 that the kits would soon be approved by the Food and Drug Administration. Wadley had ordered the tests much earlier, in November 1984. The first shipment of 2,000 test kits arrived at Wadley March 7, followed by many additional shipments.
The trouble began on March 11 when a man gave blood at a mobile bus set up at his office. Screened by donor technicians, his blood, made into three different blood products, eventually found its way into James Kilgore’s veins. But despite the fact that more than 2,000 test kits were in its possession, Wadley apparently didn’t use them to test the blood Kilgore received.
Instead, according to allegations in a lawsuit filed by James Kilgore and his wife against the blood bank, several doctors, and Methodist Medical Center, Wadley used the tests to evaluate its own AIDS test, a product of its research. For almost ten years, Wadley had run an interferon lab, set up on the heels of discoveries that the blood-derived substance might prove to be the “magic bullet” that would cure cancer. A Wadley doctor had developed a test designed to detect AIDS carriers by measuring their interferon levels. But Wadley didn’t know if the test worked and was desperate to find out. Whoever could get an accurate test on the shelves the fastest would capture the market.
Was Wadley looking to the bottom line? With an estimated potential market of $50 million annually, the test kit Wadley scientists had developed would go a long way toward putting the almost insolvent institution back on its feet.
Ironically, tragically, its test didn’t work. Ironically because after ten years of research, the researchers discovered that many healthy people have elevated levels of in-terferon. Tragically because AIDS-tainted blood was given to patients while Wadley delayed testing outgoing blood. In 1986 the interferon lab was dismantled.
It wasn’t until April 22, 1985, six weeks after Kilgore received blood, that Wadley began screening all incoming blood, and even later before all of its inventory was tested. Wadley officials apparently knew six months after Kilgore received the blood that the donor was infected. But it wasn’t until almost nine months after that discovery that the blood bank informed Kilgore. Had Wadley notified him sooner, Kilgore’s wife might not have been infected.
Through a public relations spokesman at Wadley, the president of Wadley, Dr. Norwood Hill, declined to be interviewed for this story despite several requests, citing pending litigation about AIDS. Ten lawsuits have been filed against the center alleging that plaintiffs contracted AIDS through transfusions of blood from Wadley. One was dropped. A jury found in Wadley’s favor in another. In one case, a judge issued an order in favor of Wadley against a non-attorney who represented herself. An eleventh suit cites mental anguish over a false positive AIDS test result that was released to a doctor. The James Kilgore suit was settled out of court for $2 million in September 1989. Seven are still pending.
In a deposition in the Kilgore lawsuit, Hill claims that Wadley did not begin testing the blood until April 22 because “we had to begin a set-up and phase-in after that time. It’s not possible to do a test that you haven’t learned how to perform.” But a representative from Abbott Laboratories, manufacturer of the test, says in an affidavit that the test used “the same laboratory and technical equipment required for Abbott’s [hepatitis] test, which Wadley had been using since 1981.” Not much training was required, in other words. Still, she offered to train Wadley technicians on March 6; they told her to return on March 12. which she did.
And Kilgore wasn’t notified of the AIDS “lookback” results until June 1986 because the procedure took many months to develop, Hill says. Wadley’s customers- doctors and physicians-’did not want to know this information.” Ironically, however, the committee Wadley formed to develop lookback procedures only met quarterly-every three months-when each day that passed could mean the difference between life or death.
Based on the amount of blood donated at Wadley in an average six weeks, some 20,000 units probably went out between March 7 and April 22. Undoubtedly, many of them were transfused after elective surgery, such as Kilgore’s. that might have been postponed. But there is no record that Wadley suggested to its client hospitals and physicians that they might want to put off elective operations requiring blood pending the implementation of AIDS tests.
And, in court documents, Wadley admits that Kilgore was infected but denies that blood from Wadley was the source of his infection. The blood bank also denies that AIDS caused his death.
In one sense, what happened to the Kilgores is a private sadness, an individual horror difficult for others to comprehend. But blood, in a strange way, is community property-a natural resource much like air and water. For thirty-eight years, Dallasites have been answering Wadley’s call, providing blood in the spirit of civic duty, with an attitude much like that reserved for military service. You do what you’ve got to do. People’s lives hang in the balance. And given the bond that exists between a community and those who control its blood supply, what happens at Wadley, despite its penchant for secrecy, is anything but private.
The AIDS epidemic is not the focus of this story; the fatal disease just happened to be the issue that brought many of Wadley’s problems into the open. It’s about an institution that for years has abused the public trust. Yes, many sick and dying people are saved with Wadley blood. But blood means more; blood means money. Though Wadley receives each pint of blood for free, it turns around and charges up to $100 per pint, one of the highest prices in the country, excluding San Francisco and New York.
And blood, in the scientific world, means power. Wadley’s raison d’etre is research, and donors provide Wadley with vast quantities of research material for free, a fact noted in the minutes of a 1985 Wadley retreat: “The main thing about the blood bank is that it is resource material for the research center. . The average citizen doesn’t realize this about the blood bank. Most people wouldn’t give their blood for research.”
No, most people give blood for those people in the plane crash, or the child bitten by a dog, or a James Kilgore-not to help a center develop patentable, profitable research products. Trading on a prestigious name, answerable to no one. the family that controls the Wadley institutes has taken profits from blood and built a personal kingdom, a medical fiefdom outside the mainstream of medicine, and so secretive that a spokeswoman even refused to reveal who was currently on the board of directors. “That’s confidential,” she snapped.
THE J.K. AND SUSIE L. WADLEY INSTITUTE and Blood Bank actually encompasses a hospital, a research institute, and a computer science center as well. A not-for-profit, tax-exempt corporation. Wadley provides most of the blood used in the Dallas area. But interviews with insiders and former employees, court papers filed in numerous AIDS lawsuits, and documents obtained by D Magazine through the Freedom of Information Act paint an alarming picture of an organization run amok, like a runaway train with no one at the controls.
Former employees of the blood bank describe scenes that might be out of Dante’s Inferno: employees so careless they threw bags of contaminated blood, splashing on walls and floor, into the foul-smelling autoclave room where unusable blood is to be burned. Blood that should have been stored at cold temperatures would be left out on counters so long it would get crusty. To save money, Wadley bought a refrigerator that wasn’t designed to hold blood; after it consistently got too hot, employees cut a hole in its top and ran cool air into it from the building’s air-conditioning ducts.
And even after Wadley implemented AIDS testing on all blood, infected units still slipped through. In 1986, a nurse was literally walking into a patient’s room at Baylor University Medical Center to infuse one unit when a frantic call came from Wadley saying that the unit had tested positive for AIDS. And a medical technician who worked three weeks at Wadley through a temporary service in 1987 has testified that she saw AIDS test results falsified.
“They were sloppy,” says one former employee, who says he was told “if you don’t like it, get another job” when he tried to improve quality control.
But “sloppy” is too generous a word. In fact, Wadley was cited for numerous violations in 1980, 1981, and 1982 and came perilously close to having its license suspended in 1986. After an inspection that lasted more than a week, initiated in response to anonymous complaints filed by Wadley employees, the Federal Food and Drug Administration issued a regulatory letter-one administrative step away from a license suspension-because blood products were stored and handled improperly and potentially could be worthless, even dangerous, to recipients. In response, Wadley issued a product recall that was kept so hush-hush that few Dallas doctors ever knew it happened. After the 1988 inspection, another regulatory letter citing “serious violations” was issued.
The attitude that seemed to permeate the blood bank percolated through the other Wadley entities as well. The cancer hospital’s reputation is so poor that few area physicians will agree to see or refer patients there.
And Wadley’s research institute has become widely regarded as a joke in the Dallas medical community because it is staffed by scientists who, for the most part, do not publish in peer-reviewed journals or attend scientific forums.
The man who ostensibly runs Wadley is Dr. Norwood Hill, son of Dr. Joseph M. Hill, the pathologist who founded Wadley in 1951. Both serve on the board of directors, where for years they have stonewalled those who see the need for changes. Obsessed by the Holy Grail of medicine-a cure for cancer-the Hills have controlled Wadley like medical Machiavellis, allowing little information in or out, easily manipulating a board of directors stacked with prominent Dallas business people.
Often described as geniuses, the father and son have long nursed big dreams. Wadley could be, would be, the Mayo Clinic of the Southwest, the M.D. Anderson of Dallas. Cancer researchers all over the world would speak the name Wadley-and Hill- with reverence.
“Norwood is a dreamer,” says one former high-ranking administrator at Wadley. “But he cannot bridge the gap between where I am and where I want to be.” Instead of taking realistic steps toward building a solid clinical research program, the Hills have consistently sought splash over substance. Over the years, Wadley has retreated into a shell of inflated egos, secrecy, and paranoia.
“It’s the strangest, closed, fearful group of people,” says another former employee, a lab director. “It’s a dreadful, dreadful place to work. They literally and figuratively bleed the community and give nothing back.”
Wadley has become the Mayo of Mediocrity. “You get the impression that Wadley is the Hill family toy,” says one former Wadley hospital administrator. “They want to have a blood bank. They want to have a hospital. They want to discover the cure for cancer. But they want to make sure everyone knows it’s because of them.”
And-like Machiavelli-they seemed to espouse the idea that the end justifies the means. After ail, we’re saving lives here.
And the Kilgores? Were they simply unlucky statistics?
WADLEY HAS NOT BEEN FREE FROM CONtroversy over the years. In 1967, Dr. J.M. Hill, Norwood’s father, was censured by the Dallas County Medical Society for announ-cing he had discovered the cure for leukemia; two months after proclaiming nine-year-old Frankie Hayes cured, the boy died. The incident smacked of a cheap publicity ploy because it, like many other such announcements, coincided with a major fundraising effort.
In the Seventies. J.M. Hill was accused of scuttling several blood drives scheduled by the Dallas Blood Center, which pays donors. And Wadley has fought off several attempts to create a community blood bank by area hospitals concerned about maintaining an adequate blood supply.
Norwood Hill became medical director of Wadley in 1968, the heir apparent. From the beginning it was clear that Norwood’s interests were not the same as those of his father. “I don’t know that Norwood ever wanted to be a doctor.” says a former Wadley administrator. “Somewhere along the line he got fascinated with computers. You could ask him the time of day and he’d direct the conversation to computers.”
In 1976, J.M. Hill retired, though he retained a seat on the board of directors, and Norwood became president of Wadley Institute. The baton was passed. Or was it?
“Norwood is the reluctant president of the institute,” says a former administrator of the hospital. “J.M. is controlling it through Norwood. Theirs is very much a father-son relationship.” The personality of the institution changed little with the handoff from dad to offspring: the Hill way is the right way. Don’t criticize; we’re saving lives here!
But there were tremors in the relationship. The elder Hill made it clear to other high-ranking managers that he thought his son spent too much time tinkering with computers. And administrators in charge of the research institute, the blood bank, and the hospital felt it was hard to get Norwood’s attention.
“You’d be talking to him and he wouldn’t seem to follow what you were saying.” says Dr. Hannis W. Thompson, former associate medical director of the blood bank. “It seemed that his mind was somewhere else entirely.”
Thompson quit in March 1988. “There were so many other interests [besides the blood bank].” Thompson says. “So many other people wanted money for their own purposes (within Wadley]. The main emphasis was developing hospital software.”
That was Norwood’s baby: Wadley was going to be the IBM of medical software. There was only one problem. After Wadley spent literally millions of dollars developing hospital and blood bank programs to market, nobody wanted them. The competitive software market had outdistanced them. While his attention was on computers, the blood banking industry was facing its biggest crisis: AIDS.
But according to people at Wadley, in the early Eighties, when it was becoming clear that the virus could wipe out the blood banking industry and Wadley Institute. Norwood Hill didn’t want to hear about AIDS. Indeed, in another AIDS-related lawsuit, Barron Powell Adams v. Wadley and Baylor University Medical Center, Wadley’s lawyers denied that Hill knew in February 1985 that AIDS could be transmitted by blood, easily two years after the rest of the medical world learned this.
“Norwood is definitely afraid of AIDS,1’ says a former high-ranking administrator. “You’d think that anyone committed to quality research and involved with blood banking would be looking for some way to make a dent on the AIDS front. But he didn’t seem to want to talk about the issue at all.”
Another employee who worked in the blood bank says there was no awareness that AIDS was a major issue. “If they were so concerned about AIDS I never got that impression,” he says. “It should have permeated our management meetings. I didn’t see Dr. Hill at a management meeting talking about it. Not once.”
That doesn’t surprise a former lab director in charge of testing at the blood bank, who says that in the several years that he was there he never saw Hill in the blood bank. “Few people had access to him.” the lab director says. “I never had a conversation with him. I could have been the janitor for all he knew.” When it came time to do AIDS testing, the lab director, supposedly in charge of all testing, says he was told nothing.
But after Hill was served with the first of many subpoenas to give depositions in AIDS cases against Wadley. the disease became all he talked about, says Thompson.
WADLEY’S GEOGRAPHIC MONOPOLY stretches across six to eight counties, with about sixty-five hospitals. Each year, Wadley makes about $16 million from blood: $1 million to $2 million of that is sunk back into the institutes-though not necessarily to improve blood service. Over the years, Wadley’s grip on Dallas has been periodically challenged by client hospitals, mostly because of Wadley’s high price, but also because in some years, the blood bank has had difficulty providing an adequate supply. That was the major reason Parkland in 1981 began drawing its own blood.
But every attempt to create a regional blood bank to get local hospitals out from under Wadley’s thumb has failed. “No doctor wants to bad-mouth Wadley,” says a former Wadley blood bank employee. “Hospitals wouldn’t organize. That would be suicide.”
As in many industries without competition, says Tom Asher, chairman of Hema-Care, a California blood products company, blood bankers sometimes grow lazy, arrogant, and non-responsive. That was vividly revealed, he says, in the AIDS crisis at Wadley and blood banks around the country. The President’s Commission on AIDS criticized the blood industry for not responding more quickly to the epidemic.
Even without an AIDS virus lurking in the nation’s collective bloodstream, blood is not a completely risk-free product. About 5 percent of all blood recipients develop hepatitis; roughly a third of those develop irreversible liver damage and die. Other reactions are possible, especially if the recipient accidentally receives the wrong type of blood. Blood must be handled with extreme care: regulations by both the FDA and the American Association of Blood Banks require strictly monitored storage temperatures, a detailed labeling and tracking system, and rigid donor screening. Even before AIDS, blood underwent a series of seven tests.
However, in terms of personal ambition and medical prestige, blood banking is low on the totem pole. “Research is more interesting to top people,” says Harvey M. Sapolsky, one of the authors of The American Blood Supply, a book printed by MIT Press. “You get sloppy. You forget about whether the truck goes out on time and the testing is done properly. It’s a tough thing to do every day.”
But patients who need blood can’t afford for someone to be asleep at the bloodmobile wheel. Though Wadley makes much of its efforts to provide a safe blood supply, FDA documents obtained by D Magazine and interviews with FDA officials revealed “serious violations” in 1980, 1986, and 1988 with the quality control of blood storage, handling, or testing.
For example, in 1986 testing showed that high percentages of the products did not meet FDA standards. On one date, 75 percent of the cryoprecipitate tested failed to pass the FDA quality control test for Factor VIII, the clotting factor needed by hemophiliacs. If a hemophiliac had used the product, it would have provided little therapeutic value and would have been potentially dangerous if he had received a cut or wound.
Platelet quality below that allowed by the FDA was an even bigger problem. Trauma or surgical patients receiving platelets significantly below potency requirements might require far more blood units than normal, thus exposing them to more risk for hepatitis and AIDS.
Wadley officials appear to have been aware of several of the problems. But they systematically ignored them. For example, after a technician complained that a cooler holding platelets was too hot, Wadley supervisors Janice Schonwetter and Raya Zerger wrote an internal memo dated February 11. 1986, stating that “we do not feel there is/was a problem with the cooler in Room 123.” However, seven days later, the FDA began a week-long inspection that revealed not only that the cooler was out of acceptable range, but that Wadley employees apparently tried to cover up the problems instead of fixing them. On some quality control charts, FDA inspectors noticed that notations indicating unacceptable temperatures appeared to have been altered.
After the inspections, Wadley initiated a “voluntary” recall, destroying from its in-house inventory at least 212 units of red blood cells and 226 units of platelets. They retrieved from area hospitals all units of cryoprecipitate and fresh frozen plasma dated prior to February 20, 1986, in order to destroy’ them. But not all of the products subject to recall could be retrieved; some had already been infused.
The recall was handled very quietly. Even Dr. Edwin A. Steane. former director of the Parkland Hospital blood bank, knew nothing about it. “It’s a very rare event to have the recall of blood.” says Steane, who is now director of blood services at the American Red Cross in Nashville. “It’s never happened at Parkland. That means that there is something very wrong over there.”
’”Norwood ran a sloppy shop,” says another blood expert. “He was accountable to no one. His board of directors should be ashamed of themselves.”
The problems didn’t end with the February inspection. On March 28, in a follow-up inspection, more than half of the blood bank’s cryoprecipitate that was tested failed potency tests.
A few of the other quality control problems included:
? One former employee in shipping says that, in the mid-Eighties, he saw blood intended for babies (which has to be specially tested and handled) sitting out on a counter where it reached 72 degrees Fahrenheit; the proper storage temperature should never be above 43 degrees. “I refused to ship it.” he says. “Someone else shipped it, then shipped it out too cold. Whatever that baby got was crap.” (It is unknown what happened to the baby. Steane says there is little way to follow up on blood recipients.)
A product incident report filed by Doc tors Hospital on November 11, 1985, re ported that the bag of blood shipped from Wadley had “gram negative rods,” or bac teria in the bag. The problem wasn’t noticed until after the blood was infused into a pa tient, who was duly charged for the blood.
Another product incident report, filed by Presbyterian Hospital and dated March 30, 1986, reported that a unit of blood had been labeled A positive when it was actually O positive. Being infused with the wrong blood type causes at the least a fever reaction; some mismatches could potentially cause a sick patient to die.
Another report filed March 26,1986, by Westgate Hospital says they had received a unit clotted with ice. One former employee says that, between 1982 and 1986, BSIs, frozen blue bars of glycol that are stored in the deep freeze and therefore much colder than standard “wet” ice, were used to cool the shipped blood. “It would put ice chunks in the blood,” says the employee. “That would render the blood worthless.” Not only that, he says, “They would use the |wet] ice for orange juice for donors instead of for shipping blood.”
In 1988 a wrong number was entered on the computer, resulting in units that were possibly contaminated by the hepatitis virus being shipped out. Six components were in fused before the mistake was caught. Another unit was shipped out before the entry was made in the computer labeling it a “self-deferral.” (Self-deferral is a confidential means for high-risk donors to let the blood bank know their blood should not be used.) And numerous products had been shipped out mistyped.
Wadley had a unique approach to the problems reported in the written product incident reports. It simply eliminated the reports in 1986. “Now the reports are verbal only,” the employee says.
But one of the most frightening problems was that, despite the fact that Wadley had the test for AIDS after early 1985, that didn’t ensure that blood testing positive wouldn’t slip through the system even after they began using it on all blood products. In both the 1986 and 1988 FDA inspections, Wadley was cited for incidents in which blood that had tested preliminarily positive for AIDS and hepatitis was shipped.
“If something tested positive, they’d make a notation in the computer, but they wouldn’t pull it from stock,” says a former Wadley employee. “If, in a crisis, they needed that [blood] type, they would erase the flag and send it out.” And sometimes, he says, the computer system would crash, remaining down for as long as a weekend. “The blood would go out anyway.”
Though a follow-up FDA inspection in August 1986 revealed “no significant problems,” there is much evidence that Wadley has still not cleaned up its act. Leigh Ann Morris-Keener, a lab technician who came to work at Wadley in 1987 through a temporary service, testified in court that she saw blood test results for AIDS and hepatitis falsified by altering the controls against which the blood to be tested was measured. Realizing that altering the controls invalidates the test, Morris-Keener testifed in Baker et al v. Wadley that she asked the lab technician: “Can you do that?” “Oh, sure, we do it all the time,” she was told.
“While I was there, there was a big discussion going on that somehow some units had gotten released that were sent to a hospital to be transfused to a newborn that later tested positive or that were indeed on hold, but somehow they had slipped through the computer,” Morris-Keener testified. She told her employer she refused to work at Wadley, quitting after three weeks. “I said there are just some things going on that I really don’t want to ethically be a part of.”
An FDA inspection in September 1988 indicated that many of the product quality control problems had improved. However, the inspectors cited Wadley for not having written “standard operating procedures,” and for continued computer tracking and labeling violations that are potentially dangerous.
Wadley is not the only blood bank that has had significant problems. Another FDA inspection revealed similar problems at American Red Cross Blood Services in Washington, D.C.. in 1987. Though the ARC received only a “Notice of Adverse Findings” letter, not the more serious “Regulatory” letter received by Wadley. the ARC voluntarily closed its testing and labeling section because it could not correct errors in its handling of blood. No such offer has ever come from Wadley.
The FDA did not suspend Wadley’s license, says Gerald Vince, director of the FDA”s Dallas district, because “there has not been a pattern to [the violations].” Vince says that Wadley’s problems were much worse in 1986. “A lot of the 1988 problems had to do with not having written standard operating procedures,” Vince says-similar, in other words, to the problems the Red Cross was having in Washington, D.C.
The results of the 1989 FDA follow-up inspection say that Wadley is still having difficulty tracking and labeling blood. In addition, Wadley recalled certain products prepared from April 1987 through March 1988-products that had tested positive for hepatitis, or had incorrect expiration dates. Wadley was cited by the FDA for not informing the agency of the recall. Employees say other problems are not detected by the FDA because Wadley knows in advance about some inspections. Though Vince says advance knowledge is “as strong a line of BS as you can get,” a donor technician who worked at Wadley in late 1988 says that new people-who would presumably make Wadley look bad to inspectors-were sent home with pay as long as the inspectors were there. “Everything was cleaned up and spotless,” she says.
As for the cause of Wadley’s many serious problems, that depends on who is telling the tale. Those who see Norwood Hill as arrogant and condescending say he simply didn’t care about the blood bank, except as a cash cow to fuel his other ambitions. Those who see Norwood as sincere, but distracted by his interest in computers, say that he chose the wrong people to oversee the facility. At the close of the 1986 inspection. Hill told the FDA he had fired four employees in an effort to improve quality.
One of those Hill blames for problems the FDA uncovered was Dr. Kurt Osther, the scientific director of the blood bank. Osther, brought to Dallas by Wadley from Denmark, was one of the few researchers who published scientific papers and attended international conferences. Hill fired him after learning that Osther had gone to trustee Herbert Hunt with a letter saying: “I have been strongly urged by Dallas area major hospitals to recommend that Dr. Norwood Hill immediately be removed from his position as Executive and Administrator over the Blood Center and that a Blood Center board immediately be developed.”
Many employees at the blood bank agree that Osther was the problem. For one thing, these employees say, Osther was from Denmark and didn’t understand how things worked in American research. He hired his wife and other friends from overseas to be his laboratory assistants, and they formed a very tightknit group. But other employees say Kurt Osther was trying in vain to make improvements.
In a deposition, Osther said he was given twenty minutes to vacate the premises and was forced to leave behind all his records and diplomas. He was later sued by Wadley for control of a quick Western Blot test, an AIDS test Wadley claimed Osther had developed while employed there. (The settlement in the suit, which one Wadley administrator said barely covered the blood bank’s legal expenses, prohibits Osther from discussing the case. He declined to comment on Wadley for this story.)
Whoever was responsible, it was a hell of a way to run a blood bank in the era of AIDS.
But Osther’s contention that hospital administrators wanted Hill out points to the tenuous relationship between Wadley and its clients. Hospitals do not test blood beyond confirming the blood type; they are one link in a long chain of trust that relies on Wadley to meet the high standards set up by the FDA and the American Association of Blood Banks. Hospitals, in fact, have little say in how Wadley is run, though each client facility has a representative on a Wadley blood bank advisory board, “It’s not like the usual advisory committee that would advise them.” says Edwin Steane. ’They advise us of what they’re doing. It’s kind of strange.”
And blood bankers at area hospitals are reluctant to criticize Wadley. Dr. Alain Marengo-Rowe, director of the Baylor Blood Bank, says that the problems with blood quality were exaggerated by the FDA, that the inspectors would shut them down if there were real problems. “If those things that are in there are serious, why isn’t Wadley closed? Why haven’t they penalized Wadley?”
But several hospital blood bankers privately admit that problems revealed in FDA documents concern them. Few are willing to speak out. Some do admit they quietly look for blood to buy from other areas, but they say it’s primarily because of price, not quality control.
“Wadley has shown themselves to be very vindictive, and I don’t want to get in a situation where we can’t [get blood],” says Ray LeClair, administrative officer of laboratory services at the Veterans Administration Medical Center. “It would be very tough to get our emergency supplies out of Wichita Falls or Waco.”
Nowadays, Norwood Hill is spending more and more of his time giving depositions in AIDS cases. One of those suits, Baker v. Wadley, has been tried in Denton County; Wadley won the suit, largely because the transfusion occurred before the test for AIDS was available. “It was too early for the jury to be willing to condemn the blood bank for failing to do something we think they should have done,” says Allen Weed, the plaintiff’s attorney. He says Wadley should have had more rigid donor screening and performed a so-called “surrogate” test for AIDS, as is done in the for-pay blood industry.
The Kilgore case, however, turned on a different issue: Wadley had the test, but did the blood bank use it?
Ellen Woodard, former head of the processing lab at Wadley, says that Wadley spent the six weeks before April 22 comparing the Abbott test with several other tests soon to be marketed to see which was the most effective. They were concerned that the Abbott test resulted in too many false positives, resulting in good blood being thrown away. But, she said. Wadley ended up using Abbott’s test anyway because it was the only one approved by the FDA at the time; they later switched to another company’s test.
According to another source, Wadley not only used Abbott kits to compare them to other manufacturers’ kits, it used them to evaluate its own AIDS test-a test that had the potential to bring in as much as $50 million a year. The test had been developed by Kurt Osther, and court documents indicate that Osther had performed as many as 10,000 ELISA tests for AIDS by April 22. Woodard says she was not aware that such a comparison was done.
The civil trial, set for February, was expected to reveal the inner workings of an institution that was pinning its hopes on a research find that would provide not only a badly needed infusion of cash, but respect as well. But on September 29, 1989, the case was settled out of court; according to a source at Methodist Hospital, a codefendant in the suit, Wadfey paid $2 million to the Kilgores, plus court costs. The terms of the settlement prevent any of the parties from discussing the case.
THE PROBLEMS WITH THE BLOOD BANK seem to seep throughout the other entities that make up Wadley Institute, including Morton Hospital. “A lot of tension and fear in the hospital has its roots in the blood bank,” says one former administrator.
When Dr. McDonald Horne arrived at Morton Hospital in 1977. he was board-certified in internal medicine. He stayed about five months.
“What I found was a small group of physicians who seemed to regard themselves and their operation very highly, but their medical treatment and medical management was inferior,” says Horne, who is now a staff hematologist at the National Institutes of Health. Of the dozen or so physicians on staff, he, the Hills, and a radiation therapist were the only American-trained doctors.
“They developed drugs in an out-building and then gave them to patients,” Horne says. “1 was flabbergasted when they gave a drug they had synthesized to a cancer patient without first testing it on animals. The woman died; she might have died anyway. But they seemed like a bunch of novices, playing with fire. I really thought it was a shoddy operation, and that their research was amateurish and dangerous. They spent huge sums of money producing interferon, but they were taking care of very sick, very complex patients without adequate support.”
Horne’s experience at Wadley was more than ten years ago, but by all accounts, little has changed. The hospital had been filled almost to its 110-bed capacity when first opened in the early Seventies; by the time Home arrived, the hospital was losing money and was attracting mostly terminally ill cancer patients eager to try experimental treatments. Today, the hospital has only fifteen to sixteen patients on any given day.
A hospital administrator hired in the mid-Eighties specifically to recruit American-trained physicians to serve on staff eventually quit in frustration. He says few Dallas doctors wanted to work at Wadley because of its reputation and the tight control exerted over it by J.M. Hill Associates, a professional corporation made up of eight Wadley doctors. (Norwood Hill is president of the corporation.) Most of the doctors were trained outside the U.S.
“Most of the foreign medical graduates were brought in because, to be frank, it was less expensive to bring them in,” says one former administrator. “They’re grateful; they like to follow the master around.”
Dr. Mark Spiegel, a gastroenterologist and chief of staff at Wadley, says he has no problems with the way patients are treated at the hospital. “They get excellent care,” he says. But the chief of staff says he admits only ’’one or two’1 patients a year to Morton; the vast majority of his patients are admitted to RHD Memorial Medical Center.
Hill had a chance to make improvements in 1983 when an expert from the Memorial Sloan Kettering Cancer Center in New York visited Wadley at the invitation of board member Lee Fikes, son of one of Wadley’s most generous benefactors. Fikes was concerned about stories he was hearing regarding the quality of research and medical care at the hospital, and he wanted an outside opinion.
The expert, Dr. Roger Herdman, reviewed Wadley’s research program, hospital, and administration. His report, dated June 10, 1983, politely rips the institution to shreds, citing “no review structure of any sort.. .a molecular biology unit which has not succeeded in obtaining an IFN [interferon] gene after two years of effort… a chemistry lab which appeared essentially inactive.. .an establishment relatively isolated from the national scientific community.”
Herdman’s letter went on to criticize the hospital staff, urging that Wadley recruit “American staff with clinical skills and drive” and enforce higher standards. “The hospital is seriously underutilized,” he said. “Surely you must see that a large portion of the staff is not occupied, and that the care intensity is not that high.”
Calling Wadley a “family sinecure,” Herdman, who is now with the Office of Technology Assessment in Washington, D.C., told D that Norwood Hill seemed insecure about the institution’s status and wanted to upgrade Wadley.
But when Herdman offered Sloan Ket-tering’s help in making changes, his report was brushed aside by the Hills. Fikes resigned from the board and eventually succeeded in getting his father’s name removed from one of the buildings at Wadley. He declined to comment.
One change did come about after Herd-man’s letter. Wadley, through the efforts of board member Charles Lee Davis, brought in a CPA named Ron Ridgers to get a handle on the institute’s finances. He recommended that the books be reviewed by an outside audit firm; Wadley hired Arthur Andersen. But Ridgers says they resisted most of his other suggestions.
“That place was a muck of secrecy,” Ridgers says. He believed the physicians’ corporation, headed by Norwood Hill, was milking the institute by keeping other doctors out and charging high fees to patients. “I saw dollars and dollars being drained out of there. Norwood was secretive about where it went.”
Finally, Ridgers recommended to the board that Norwood Hill be removed from his job. After a heated board meeting, a vote was taken. Norwood won; Ridgers quit.
But the problems persisted, recognized even by staff members who held a retreat in April 1985 to discuss the malaise that had settled over the institute. A memo circulated after the retreat, detailing the discussions, indicates that the staff knew it had a serious image problem, and that drastic changes had to be made.
Again, little was done. A search was commenced for a new chief of staff, but the candidates never quite met Norwood Hill’s criteria. “He was looking for God or his superior,” says one administrator. After five months, the search was dropped. The hospital continued its slide into near-insolvency, putting an ever-increasing strain on the institute’s budget, which is funded largely by the blood bank.
The continued financial problems leave dim hopes that the Wadley Institute can be saved intact. In several of the last audits, the reports have concluded with the notation that “We’re not sure you have a going concern.” The facility now has a for-profit subsidiary that allows it to develop products in tandem with Phillips Petroleum Co. But it will probably be years before any research pays off enough to pump money back into the hospital and blood bank. “They’re buying time; they’ve been buying time for years,” says a former manager.
Periodically, members of the board of directors have pushed for changes. But directors’ meetings inevitably turned into “dog and pony shows” with the Hills trotting out promising research finds and resisting the trustees’ attempts to address the financial problems. “What do they need to know that for?” Norwood Hill asked another administrator. “Don’t they know we’re trying to find a cure for cancer here? Why don’t they stick to raising money?”
In 1986, two trustees-oilman Hunt and Bob Chilton. president and CEO of Chilton Investments-quit, frustrated by the Hills’ resistance to the board’s recommendations. “They did demand improvements,” an administrator says. “But Norwood always had a reason he couldn’t do it. They got tired of it.” Mary Kay Ash. who declined to comment, is one of the few remaining Wadley board members. According to one administrator, empty board seats often went unfilled for years.
The Nineties inevitably will bring drastic changes to Wadley. Blood banking is being altered dramatically by consumers’ demands tor autologous (self) and designated donations. And J.M. Hill is in his eighties. “The bottom line is: J.M. created it,” says an administrator. “Now, when J.M. dies, Norwood may find himself in a corner all alone.”
One former administrator gets the feeling that the Dallas medical community is playing a waiting game. “The hospital is slowly dying. Research funds are slowly drying up. Are people sitting and waiting until Wadley gets desperate enough?”
He thinks he has a solution: “It would be a good idea to sell the blood bank to a nonprofit corporation made up of Baylor, Parkland, Methodist, and other hospitals who would oversee it and hire professional management,” says a longtime Wadley employee. “But that would be taking Norwood Hill’s toys away. The institute would fold without the blood bank.”
Without the blood bank, there would be no research, no hospital, no computer science center. No more chances to find the magic bullet. No more opportunities to leave the Hill mark on medicine. “His father started the dream of finding a cure for cancer,” says one former administrator, “but the dream has passed him by.”
But Norwood Hill shows no signs of giving up. Though the computer science division has spent millions on developing software- and so far has sold it to no one-Wadley announced a joint venture with Honeywell to document and market their computer programs, despite the fact that other software companies are far ahead of them.
“They’re chasing a dream again,” says a former administrator with an exasperated sigh, “but Wadley’s the place you chase dreams.”
THE AVOIDABLE DEATH OF JAMES KILGORE
March 7, 1985: Wadley receives the first shipment of ELISA tests to screen blood for the AIDS virus.
March 11: Donor “M” gives blood at a mobile site at his Dallas office. His blood, however, is apparently not tested, instead of testing blood being shipped out to patients, Wadley researchers use the ELISA tests to evaluate its own AIDS test.
March 12: “James Kilgore” undergoes open-hean surgery. To stop massive bleeding, he is given seventy-three units of blood, including a unit from donor “M.”
Early fall: Donor “M” again gives blood. This time, his blood is tested. Wadley discovers he tests positive for AIDS.
June 1986: Kilgore is notified that he received blood from a donor who later tested positive for AIDS. A blood test reveals that Kilgore is infected. His wife’s blood also tests positive.
July 9, 1988: Kilgore dies.
September 29,1989: Kilgore’s family settles out of court for $2 million from Wadley. -G.W.
DMAGZ121989-081_Article_001_Text_001BLOOD WILL TELL-BUT HOW CAN YOU?
Is Wadley blood safe? No. Not completely. No blood, no matter how well tested and screened, is 100 percent safe. And if it’s not well tested, screened, and stored, then the chances of getting a blood-borne disease from a transfusion increase dramatically.
Interestingly, most of the sources for this story, when asked if they would receive Wadley blood, said yes-but usually with some hesitation. Hannis W. Thompson, former associate medical director for Wadley,said, “Well. yes. Iflcouldn’tget blood from Kansas or somewhere where it’s safer.” Ellen Woodard, formerly in charge of blood processing at Wadley, said, “I hesitate to accept any blood. No matter how much you test it. it only gives you a higher degree of safety. It is dangerous to take blood. But if I had to, I would certainly take it from Wadley.”
There are ways to hedge your bet. Obviously, if you’re severely injured in a car wreck, take the blood wherever it comes from and don’t worry about it. But if you’re having elective surgery, or your doctor suspects you may need surgery in the next year or so, you can give blood to yourself. It’s called autologous giving and every blood bank in town (Parkland has the second-largest blood bank behind Wadley, and it has a very good reputation: Presbyterian also has its own small bank) and most major hospitals in the area will accept your blood and store it for you. Your own blood, obviously, is the safest you can get.
Another option is directed giving. That means you direct the hospital where you’re having the transfusion to give you only the blood that has been donated by people you have asked to donate. You probably have a pretty clear idea whether your Aunt Martha is an intravenous drug addict or your brother is a practicing homosexual. Essentially, you screen your own donors.
Just as a further precaution, be sure to tell your doctor that if it ever comes down to it, you are not to receive blood unless death or other severe medical complica tions will result without transfusion. It’s your life. You should have a say in whose blood goes into your veins. -J.P.
Related Articles

Local News
As the Suburbs Add More People, Dallas Watches Its Influence Over DART Wane
The city of Dallas appears destined to lose its majority of appointments on the DART board. How will that affect the delivery of public transit in the future?
By Matt Goodman

Home & Garden
A North Haven Gardens Coach is Helping You Reap What You Sow This Spring
Seasonal tips from North Haven Gardens' Kay Nelson.
By Jessica Otte
Arts & Entertainment
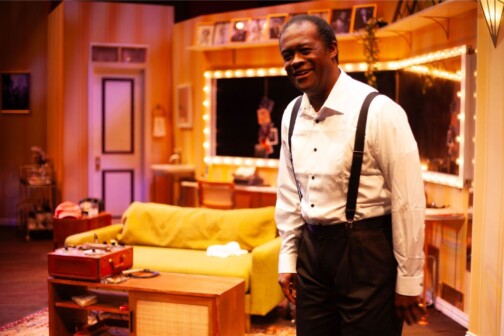
WaterTower Theatre Invites Audiences Backstage for an Evening with Louis Armstrong
Terry Teachout’s first play, SATCHMO AT THE WALDORF, shares details about Louis Armstrong after one of his final shows.
By Brett Grega