THE PATIENT is lying inside what resembles a giant thermos bottle. She is experiencing no pain-in fact, no sensation at all. A magnetic force 3,500 times that of the earth’s magnetic field is swirling harmlessly inside the “thermos.” The doctor is using the device to take pictures of the patient’s brain to locate a deadly tumor that has escaped detection by more conventional testing. The device photographs not only bone structure but also soft tissue with a clarity never before achieved. The procedure will aid in the attempt to save the patient’s life. It is known as Magnetic Resonance Imaging (MRI) and has been called a window to the body. Some MRI machines are so powerful that they can see cells in their living state inside the body. Many scientists think that Magnetic Resonance Imaging will change the fundamental practice of medicine. If so, the Dallas medical community will find itself at the very leading edge of this new technology.
Less than three of the 100 machines in the United States are in Dallas, but this is only one example of how the city is being recognized around the world for its medical advances. Dallas’ ability to attract both public and private research endowments and its commitment to building state-of-the-art medical facilities have lured some of the country’s leading scientific investigators here. Two are even rumored to be candidates for the next Nobel Prize.
The Dallas area has a total of about 50 hospitals, 4,000 physicians and a medical school that is earning a reputation as one of the best in the nation. The University of Texas Health Science Center is ranked by national peer review among the top 15 U.S. medical schools, along with Johns Hopkins, Harvard, Duke, Yale, Columbia, Stanford, UCLA and Pennsylvania. The LIT Health Science Center has an annual research budget of $37 million, about $7 million of which comes from private sources, and the balance from federal and state budgets. Its government support represents one-third of all such medical school funding for the entire state.
Baylor University Medical Center has the fifth largest number of patient beds for general voluntary hospitals in the United States. It is one of Texas’ few hospitals (other than those with medical schools) with a substantial research budget of $1.2 million, a figure that is expected to climb to $35 million by July 1985. Baylor has recently established the Baylor Research Foundation committed to raising some $10 million by 1990 for in-hospital research. “Ultimately,” says Boone Powell Sr., senior consultant to the Baylor Medical Center Foundation, “the new foundation will support 10 to 15 specific disease-related institutes, each with an annual budget of about $3 to $5 million.”
The Dallas Veterans Administration Hospital receives about 63 percent of its $4 million research budget from the VA and 37 percent from federal grants. It gets more than 2 percent of the national $150 million VA research budget and has just been designated by VA Central office in Washington, DC, as a schizophrenia research center.
But major advances aren’t confined to the largest of Dallas’ hospitals. Wadley Institutes has a research budget of about $3.5 million, almost all of which is from private sources, with less than 10 percent of its support from the government. It was the first to treat patients with the cancer-fighting drugs L-asparaginase and Cisplatin and also the first in the United States to manufacture another cancer-fighting drug, In-terferon. Methodist Medical Center, which performed the city’s first multiple organ transplant, has been designated a Level I Trauma Center by the American College of Surgeons and the Texas Department of Health (one of only two private hospitals in the state to receive this designation). Presbyterian Hospital is pioneering research in in-vitro fertilization and sleep/wake disorders.
The accomplishments of the Dallas medical community have not gone unnoticed by the scientific world. Dr. Michael S. Brown and Dr. Joseph Goldstein at the University of Texas Health Science Center have received a number of international awards for their work in determining how body cells process cholesterol and how an inherited defect in this process can lead to heart attacks. Brown directs UTHSC’s Genetic Disease Center, and Goldstein heads the Department of Molecular Genetics. Their work has earned them the New York Academy of Sciences Award in Biological and Medical Sciences, the Gairdner Foundation International Award (the highest scientific award in Canada) and the Lita Annenberg Hazen Award for Excellence in Clinical Research.
Dr. John S. Fordtran, chief of internal medicine at Baylor University Medical Center, is a co-recipient of the King Faisal International Prize in Medicine, Saudi Arabia’s highest honor, for his part in research on diarrhea and related diseases. His work is credited with helping save the lives of more than 5 million children who would have died each year in underdeveloped countries from dehydration caused by cholera and chronic diarrhea.
Doctors at the Dallas VA Hospital have earned the VA’s distinguished William S. Middleton Award four times since 1960 [more than any other VA hospital]. Dr. Roger H. Unger received the award for his work in diabetes; Paul A. Srere, PhD., for noted biochemical accomplishments; and Dr. Sami I. Said for hormone research. Kosaku Uyeda, PhD., won this year for outstanding research in the biochemistry of carbohydrate metabolism in the liver.
The Dallas medical community is both a tightly knit network of relationships and facilities and a series of highly distinct groups focusing upon areas of specialty which, to a large degree, reflect the collective skills and attitudes of the scientific staffs at each institution. Wadley Institutes, for example, specializes primarily in cancer and blood-related diseases. The VA concentrates upon psychological and gastrointestinal disorders. Presbyterian Hospital focuses upon maternity, eye surgery, arthritis, pulmonary and physical medicine, as well as diseases of the heart. Methodist Hospitals research heart, kidney and liver diseases in addition to trauma care. Both UTHSC and Baylor organize their research around disease centers or institutes. Baylor focuses mainly upon heart disease, cancer, arthritis, digestive diseases and infectious diseases. UTHSC has eight centers, that are devoted to cancer, genetic diseases, reproductive biology, human growth, heart research, nuclear medicine, human nutrition and rheumatology.
Leaders of these institutions agree that the future of medicine rests in biomedical technology, and they compete vigorously for funds and talent to pursue major breakthroughs in health care. The research projects outlined below are only a small sample of hundreds of current investigations. Some procedures will not be available to the general public for several years, while other techniques are already saving lives.
UT Health Science Center
THE UNIVERSITY OF Texas Health Science Center at Dallas serves as an undergirding force in the local medical community. It was founded in 1943 as Southwestern Medical College, became part of the University of Texas system in 1949 and was designated a health science center in 1972. Today it embraces a 60-acre campus on Harry Hines Boulevard and includes the Southwestern Medical School, Southwestern Graduate School of Biomedical Sciences and the School of Allied Health Sciences. The institutions have a threefold mission-education, research and patient care.
In addition to its ranking among the top 15 medical schools in the country, UTHSC is fifth in the number of faculty members who are included in a listing of the 1,000 “most cited” scientists in the United States. Six faculty members have been elected to the National Academy of Sciences, perhaps the highest medical honor in the country. In 1974, Dr. Samuel McCann, chairman of the UTHSC physiology department, was considered for the Nobel Prize for his discovery of chemicals that travel from the brain to the pituitary gland and instruct it to secrete the hormones that regulate growth, ovulation and other sexual functions as well as thyroid stimulation, metabolism and even our reactions to stress.
OTHER POTENTIAL CANDIDATES for the Nobel Prize are Dr. Michael S. Brown and Dr. Joseph Goldstein, who have discovered the dysfunction that causes the body to build up dangerous levels of cholesterol-the breakthrough that has already earned them three international awards. Goldstein and Brown identified the process by which cells take up the cholesterol they need to build their outer membranes. The cells behave like islands in a flowing stream. When an island (cell) needs cholesterol to build its outer walls, it intercepts a “barge” full of low-density lipo-proteins (LDL), which contain cholesterol. The cell takes in the LDL through LDL receptors on its surface. Once inside, the LDL is broken down by the cell, and the cholesterol is extracted to use in the building process. When the cell has enough material, it will shut its dock doors, preventing the LDL from being absorbed. When LDL cannot enter the cells, its load of cholesterol accumulates in the bloodstream like a traffic jam, eventually clogging the arteries and leading to heart failure.
In their studies of young children who were dying of heart attacks as early as age 7, Brown and Goldstein discovered that a genetic alteration in the LDL receptors on the surface of the cells prevented the LDL from being absorbed and caused the lethal buildup of cholesterol. As a result of their findings, 6-year-old Stormie Jones was quickly diagnosed at UTHSC as having the cholesterol disease, and became the world’s first heart and liver transplant recipient. Had she not lived in Dallas, she might not be alive today. There were only two other centers in the country equipped to diagnose her problem.
DR. JONATHAN UHR, chairman of microbiology at UTHSC, and Dr. Ellen Vitet-ta, professor of microbiology, along with other team members, have developed a cancer-fighting technique that, if successful in humans, could achieve permanent remission of the disease in patients with certain kinds of cancer. In their studies of mice, Uhr and Vitetta have found they can eradicate 99.9 percent of the tumor cells in the bone marrow of the rodents by using a powerful poison cocktail containing ricin. The ricin drug is attached to an antibody which, when injected into the marrow, can recognize, seek out and destroy only the cancerous cells, leaving healthy ones intact. All of the cells necessary to repopulate a human body’s blood cells are manufactured in the bone marrow. If this marrow can be removed from a patient, cleansed of cancer cells and later transplanted back into the patient’s body to produce healthy cells, permanent remission of the disease might be achieved. While human research is still in its early stages, and many difficult problems in the technique are yet to be overcome, it does offer encouragement for the future.
Space Lab Biology and Down-To-Earth Nutrition
UTHSC SCIENTISTS MAY be instrumental in solving the problem of obtaining and purifying quantities of islet cells that are used in the treatment of diabetes. Dr. Drew Gaffney will supervise a series of cardiovascular experiments aboard NASA’s Spacelab when it lifts off in January 1986, with the goal of refining raw biological materials into effective pharmaceutical products. The weightless environment of the Spacelab, a self-contained research facility on the Space Shuttle, has proven to be ideal for successfully purifying live insulin-producing beta cells needed by diabetes investigators.
For related research, Dr. Dan Foster, professor of internal medicine at UTHSC, has received the Banting Medal, the highest honor for research in diabetes. Dr. Roger Unger, a professor of internal medicine at UTHSC as well as senior medical investigator at the Dallas VA Hospital, has also received the award, making UTHSC one of the only two medical schools with two Banting prize winners on staff.
DR. SCOTT M. GRUNDY, who is the director of UTHSC’s Center for Human Nutrition and internationally renowned for his work as a nutritionist, has discovered that mono-unsaturates (such as olive oil) may be better than polyunsaturates, when used in the diet, can significantly lower cholesterol levels in the body below that of saturated fats such as those found in meat, egg yolks, butter and cream. Mono-unsaturated fats may even have certain cholesterol-lowering advantages over polyunsaturates, according to Grundy.
ONE OF THE most talked-about research projects at UTHSC is Magnetic Resonance Imaging. The school owns two of the three MRI machines in Dallas (the other is at Baylor). Dr. Ray Nunnally, director of the Biomedical Magnetic Resonance Center and MRI Clinical Unit at UT Health Science Center, explains that the powerful imaging devices can observe the flow of body fluids, see a swollen arthritic knee shrinking after treatment, watch a growing embryo inside a mother’s womb or monitor the brain as it throbs in rhythm with the heart. It is even capable of photographing the heart in three dimensions.
Unlike older scanning methods such as the CAT Scan or PETT, MR] uses no X-rays or ionizing radiation. A harmless magnet and a radio frequency energy that’s about one billion times weaker than a light bulb are the active elements of the system. The patient lies inside the opening, surrounded by the magnetic field. Under the magnet’s powerful influence, particles inside the atoms of the human body behave like tiny, spinning bar magnets. They align themselves with the strong magnetic field surrounding the patient. When struck by radio waves, which cause vibration, the particles resonate with various “tones” of energy. The resonance of individual elements at different frequencies allows sensitive imaging instruments to measure and display the elements as a total image reconstructed from computer data on a viewing screen.
“MRI should be able to identify kidney, lung and liver cancer, as well as the size and location of an internal injury,” Nunnally says. “It can also depict blood vessels without the use of contrast agents and can show moving body parts such as the heart without excessive blurring of the image.” If MRI fulfills its promise, it will diagnose stroke and other diseases caused by reduced blood supply to the brain, detect buildup of plaque in blood vessels and determine the extent of damage to muscle tissue in heart attack victims. It will also monitor the success of organ transplants and help doctors evaluate patient response to drug therapy.
Baylor University Medical Center
BAYLOR IS ACTIVELY using MRI to help doctors make critical diagnoses. The Baylor machine is powered by a 1.5 Tesla (15,000 gauss) magnet. In some cases, it has detected brain tumors and breast cancer before symptoms occur.
“We are a clinically based health care institution,” says Baylor University Medical Center President Boone Powell Jr. “Our mission is to take care of patients.”
Dr. Steven E. Harms, who heads Baylor’s Special Imaging department, says, “I believe that MRI technology will one day be considered as important as the discovery of X-ray technology and antibiotics.” Harms was one of the first to achieve three-dimensional body displays with MRI. The MRI data, combined with other scanning devices, also enables Harms to make exact plaster replicas of damaged bones and joints. This provides the surgeon with a tactile model that he can study before performing an operation.
Harms and his team have now intensified MRI’s ability to receive radio frequency signals and have developed an imaging technique to obtain signal images of entire portions of a given area of the body at once, rather than slice by slice. This will enable doctors to gather more information about a patient in a shorter test period.
BAYLOR MEDICAL CENTER is a leader in the use of laser light beams for surgical and other kinds of treatment. Baylor was the fourth hospital in the world (Dallas’ Wadley Institute was fifth) to acquire the CO2 laser in 1974. Today, Baylor has 70 doctors on its laser team-more than twice the number at Harvard Medical School.
Dr. Billie Aronoff and Mel Judy, Ph.D., are now successfully using laser light to treat certain forms of cancer in some patients, including liver, spleen, colon, breast, vascular tumors, sarcoma and others. One application of laser light is photodynamic therapy, a process by which cancer cells are selectively destroyed by red light from a dye laser. “The laser is not a miracle cure for everything,” Aronoff says, “but if used correctly, it can enhance a patient’s quality of life.” According to Dr. Aronoff, a patient is injected with a special drug, which makes the patient light-sensitive. After 72 hours, 90 percent of the drug will concentrate only in cancer cells. When the patient is exposed to the ultraviolet light, the tumor thus becomes a brightly lighted target. When struck with red light from the special dye laser, oxygen in the diseased tissue explodes, destroying it. Because the free-electron laser can focus on infinitesimal points deep inside the body, photodynamic therapy may be an important cancer treatment of the future.
IN 1975, TWO researchers, George Kohler and Cesar Milstein of Great Britian, discovered that by fusing a normal human antibody-producing cell with a specific type of cancer cell (myeloma) extracted from a mouse, they could produce a third hybrid cell in the laboratory. This cell, when injected into the rodent, can recognize and seek out the cancer cells from which its diseased parts originated, much like a homing pigeon finds its way back to its point of departure.
This meant that doctors, for the first time, could manufacture cells in the laboratory that might be able to recognize different kinds of cancer when injected into an organism. Eventually, they could develop human-to-human hybrid cells, attach cancer-killing agents to them and send them into the body like magic bullets to knock out the disease. The process, called Monoclonal Antibodies, is a breakthrough in methodology, according to Dr. Marvin J. Stone, who heads the Sam-mons Cancer Center at Baylor Medical Center. But for now, it is more useful in helping doctors learn more about the appearance and behavior of tumor cells than as a cancer-fighter.
DR. JOHN S. FORDTRAN, Baylor’s chief of internal medicine, helped develop a solution that restores fluids to victims of severe diarrhea. Before this discovery, dehydration had been a leading cause of death among young children in underdeveloped countries. Baylor is a major center for the study of chronic diarrhea, one of only a few such centers in the world.
Wadley Institute
IN 1978, THE American Cancer Society allocated $2.4 million-the largest research grant in its history-toward the study of Interferon. By 1980, it had increased its Interferon grant allocations to nearly $7 million. Interferon, a natural protein produced by cells when they are invaded by a virus, is one of the most promising cancer-fighting drugs. But until now, the scarcity of the drug has hampered scientists in their research efforts.
Wadley Institute of Dallas was the first, and is now one of the largest, producers of Leukocyte Interferon in the United States, and was also the first to show responses to Interferon in patients with leukemia in 1977. More recent patient trials at Wadley suggest that Interferon may be effective in treating several different forms of cancer, including melanoma, lymphoma and multiple myeloma.
Dr. Amanullah Khan, chairman of the department of immunotherapy at Wadley says, “We believe that by combining two of the three types of Interferon and/or treating the patient in combination with chemotherapy, we may obtain improved results. Studies are under way in both of these areas. But one of our major difficulties has been in manufacturing and purifying enough Interferon to intensify our investigations.”
But Wadley may be upon the threshhold of solving that problem. “We believe the new genetic technologies will make virtually unlimited supplies of Interferon possible,” says Dr. Norwood O. Hill, president of Wadley Institutes.
Dr. Arthur P. Bollon, director of Genetic Engineering and chairman of the department of Molecular Genetics at Wadley, has just reported in the Proceedings of the National Academy of Sciences that he and his team have found a way to greatly improve the isolation (and therefore the manufacture) of human Interferon genes. From those studies, Bollon has isolated two new human Interferon genes that have never before been identified and used for manufacture.
OTHER RESEARCH PROJECTS at Wadley include a new technique that can predict with about 90 percent accuracy whether a patient’s cancer cells will be resistant to a certain drug. It can also predict with 60 to 70 percent accuracy whether the patient may have a positive response to the drug. The new test, called stem cell assay, will help doctors avoid ineffective and unnecessary toxic drug treatment.
Dr. Gordon L. Dorn, chairman of the department of microbiology at Wadley, has developed a faster testing device for infectious diseases. The device, called the Isolator, is a means of detecting bloodstream infections and is now being marketed worldwide by the E.I. DuPont Co. Dorn explains that 30 to 70 percent of all cancer patients die from infectious diseases, rather than from the cancer itself. One of the most serious of these is sep-ticemia. Dorn says that about one-fourth of those with septicemia die because of a delay in diagnosing the infection. The Isolator, which looks similar to a stoppered test tube, quickly detects the specific microorganisms involved in the disease so that appropriate antibiotics may be given before acute infection occurs.
Methodist Medical Center
METHODIST MEDICAL CENTER, a regional leader in transplantation, was the first private hospital in the city to offer an organ transplant program. Since the program began in June 1981, Dr. Richard Dick-erman and his team of nephrologists have transplanted more than 250 kidneys with a success rate of 87 percent. The first liver transplant in Texas was performed at Methodist in October 1984, and a pancreas transplant and a pancreas/kidney transplant have also been performed there.
Of the 250 kidney transplants performed at Methodist since 1981, the mortality rate is 3 percent. Eighty-seven percent of the transplanted kidneys are still functioning.
VA Hospital
MANY ULCER PATIENTS and some physicians believe that the symptoms of peptic ulcer disease often occur shortly after a stressful life event. In his studies of peptic ulcers at the VA Hospital, Dr. Mark Feldman has shown that peptic ulcer patients may not have significantly more stressful life events than other people. The peptic ulcer victim, however, “perceives” significantly more negative events in his life. Dr. Feldman believes that peptic ulcer patients may be more vulnerable to stress than others and may have a reduced ability to cope with stress. VA studies have shown that ulcer patients have a 50 percent chance of also being clinically depressed. Of that group, some 60 to 90 percent will have recurring ulcer problems.
MICHAEL VASKO, PH.D. hopes to help the scientific community broaden its knowledge of the mechanisms involved with pain so that better pain-relief methods can be developed.
“In our laboratory, we are attempting to study which neurotransmitters (substances released from nerves that communicate with other nerves) are important in the pain pathway between the brain and the spinal cord. We are also looking at how they interact to modify incoming pain signals,” Vasko said.
THE SCHIZOPHRENIA RESEARCH Center at the Dallas VA Hospital, in collaboration with the department of psychiatry and the Nuclear Medicine Center at UTHSC’s Southwestern Medical School, is using advanced computer imaging techniques (or brain mapping), to see whether abnormal blood flow exists in the brains of schizophrenic patients. They have found that some patients characterized as paranoid schizophrenics display decreased blood flow in the area of the brain involved in higher cognitive function (the frontal lobe). Using the computerized brain maps, the researchers can locate the area of the brain where the dysfunction responsible for schizophrenia occurs and use the information to make better diagnoses and to develop more rational approaches to treating mental disorders.
Presbyterian Hospital
About a year ago, Presbyterian Hospital of Dallas opened its In Vitro Fertilization/Embryo Transfer Program to help couples overcome infertility and have families that are genetically their own.
In the In Vitro (“in test tube”) fertilization process, doctors first give the woman a medication that they hope will cause the ovaries to produce two or more mature eggs. The Presbyterian team then monitors the maturing eggs through ultrasound and other tests to determine the precise moment when maturation occurs. The eggs are retrieved by a minor surgical procedure and, in most cases, at least one egg is recovered. The eggs are then taken to a highly specialized culture laboratory. At the appropriate time, they are fertilized by the husband’s sperm. Ater two days, the fertilized egg is transferred to the woman’s womb. Now, both doctors and the couple must endure an emotional two-week wait to determine whether a pregnancy has been achieved. At any time, something can go wrong. Under some circumstances, the woman’s brain will inexplicably send a message to her ovary to prematurely release an egg.
Dr. James Madden, one of four members of the In Vitro Fertilization Program at Presbyterian, is studying ways to override the brain messages and cause the ovaries to produce the eggs when needed. “If we can achieve this, it will be a major breakthrough,” says Dr. Madden. “We are very optimistic that this new technique several years from now, result in routine pregnancies by In Vitro Fertilization.”
“There is a sacredness about human life,” said Madden. “When we are dealing with a human embryo, we must be patient, and we must approach all of our studies with forethought, reservation and a great reverence.”
Related Articles

Local News
As the Suburbs Add More People, Dallas Watches Its Influence Over DART Wane
The city of Dallas appears destined to lose its majority of appointments on the DART board. How will that affect the delivery of public transit in the future?
By Matt Goodman

Home & Garden
A North Haven Gardens Coach is Helping You Reap What You Sow This Spring
Seasonal tips from North Haven Gardens' Kay Nelson.
By Jessica Otte
Arts & Entertainment
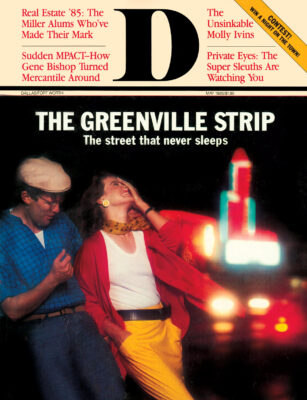
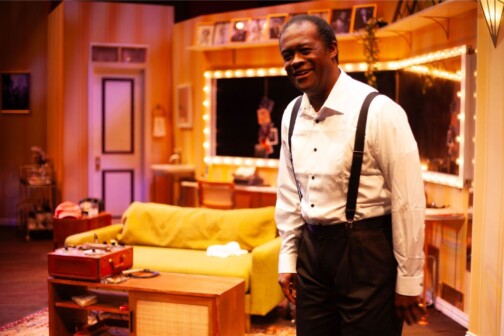
WaterTower Theatre Invites Audiences Backstage for an Evening with Louis Armstrong
Terry Teachout’s first play, SATCHMO AT THE WALDORF, shares details about Louis Armstrong after one of his final shows.
By Brett Grega