Reporting on the COVID-19 pandemic in North Texas over the past several months, I kept hearing different iterations of the same refrain: The disease has highlighted the needs we already knew were there and sped up changes that were already in motion. COVID-19 has illuminated the best and worst parts of healthcare in the United States, shining a light on inequity while spurring new ideas and improving access to care and efficiency.
But crisis breeds innovation, and the interruption of services in some sectors of the industry has led to changes in the very way healthcare is delivered. Telehealth has become the norm, allowing those who don’t have transportation or childcare or who fear for their health to see the doctor while staying at home. The way physicians are being paid could also be changing. In North Carolina, Blue Cross Blue Shield is paying independent primary care physicians up front for each patient, rather than giving them incentive to run unnecessary lab work or imaging.
Many physicians in Texas are pushing for a similar seismic shift, which seems almost inevitable. With uncertainty taking hold of the future of industries of all types, I find hope in the spirit of the healthcare community in North Texas, which remains steadfast in its commitment to serve, grow, and constantly improve. In D CEO’s special Healthcare Annual, we also hear from a diverse group of hospital leaders about how they are persevering and thriving through the worst health crisis we’ve seen in decades.
A $52 Billion Economic Force
Dallas-Fort Worth’s wide-ranging healthcare industry represents about 15 percent of the local economy.
The healthcare industry in North Texas is diverse, growing, and innovative, and its economic impact is as varied as it is massive. Health systems, hospitals, outpatient clinics, real estate, pharmaceuticals, medical devices, health tech, insurance, and other subsectors represent about 15 percent of the regional economy—or $52 billion, according to the Dallas Regional Chamber. Despite the pandemic, area healthcare companies and nonprofits will continue to play a significant role in the economy.
Employment
Prior to the pandemic fallout, the Bureau of Labor Statistics reported that education and healthcare represented 475,000 employees in Dallas-Fort Worth, up from 350,000 in 2010. The growth rate for education and healthcare hovered around 4 percent before COVID-19. Healthcare practitioners (which doesn’t include social workers, community health workers, health educators, and support staff) represent the seventh-most populous industry with 676,860 workers in Texas. Healthcare practitioners have the highest median salary ($78,470) of all the top occupations. Health support professionals add 543,430 workers to the Texas economy.
Hospitals in North Texas have a marked impact on the economy, too. In addition to jobs in hospitals, they create construction, consulting, real estate, and other positions. There are 90 hospital members in the Dallas-Fort Worth Hospital Council that have a $14 billion impact on the economy and add 265,000 jobs statewide. According to a 2017 report, member hospitals in the Dallas-Fort Worth Hospital Council accounted for 126,385 jobs in hospitals, 7,000 construction jobs, and 161,754 jobs created in other businesses. Member hospitals paid their employees $10.6 billion. They also paid $353.4 million for construction personnel and $7.5 billion in secondary labor costs. It all adds up to $18.4 billion in labor impact generated by hospitals in North Texas.
“Because of all the companies that are located here, from name brands to other lesser-known companies, DFW is really strong,” says Duane Dankesreiter, senior vice president of research and innovation at the Dallas Regional Chamber. “Even though you often don’t hear about some corporations, they make products you use on a regular basis, and they are embedded into the fabric of healthcare across the region.” Additionally, healthcare is a job-creation machine, Dankesreiter says. “For every healthcare job, several jobs are multiplied around it, which is key for why healthcare is so important to the region.”
Of the 25 largest employers in North Texas, six are in the healthcare industry. Texas Health Resources (the fourth-largest, with 19,000 employees), Baylor Scott & White Health, UT Southwestern, Parkland Health and Hospital System, Medical City Healthcare, and Cook Children’s Hospital all take a spot on the list. North Texas is also home to drug distribution giant McKesson, the seventh-largest company in the country, with annual revenue of $208 billion.
Innovation
Healthcare has been a major driver of new devices, pharmaceuticals, and technology in the region. “DFW has established itself as a robust region that is innovating in the healthcare field,” says Dr. Hubert Zajicek, co-founder and CEO of Healthcare Wildcatters. “Our strengths are several strong hospital systems, a top-four metro area by population, continued strong growth of talent, and several rapidly growing universities.”
Based in downtown Dallas, Health Wildcatters is an accelerator that pairs cohorts of healthcare entrepreneurs with mentors and provides them with funding. The organization also hosts an annual competition where cohort members pitch in front of an audience of potential investors; since its founding in 2013, 68 accelerator graduates have raised $70 million in funding.
In June, Dallas-based biotechnology company (and Health Wildcatters alum) Lantern Pharma raised $26 million in a public offering of its AI machine learning, which identifies patients who will benefit from targeted oncology therapies. Southlake’s Onconano, which was launched by UT Southwestern researchers, won $15.4 million in funding from Cancer Research Institute of Texas in 2019 for its work on the treatment of HPV.
DFW has had several recent healthcare innovation wins, including Vivify’s acquisition by Optum, Axxess Healthcare’s continued growth, and significant pharmaceutical growth with companies like ZS Pharma and Reata. “I think the fact that companies can grow here is not an outlier anymore, it is established,” Zajicek says. “The next question will be if we can retain companies during continuous growth after the respective acquisitions, or grow healthcare companies to Fortune 500-size.
“I believe we can now,” Zajicek continues. “Three of the Top 10 DFW-based companies are healthcare-related: McKesson, Tenet, and Kimberly-Clark. It signifies that we’re not talking about an aberration anymore, but rather a strong component of our regional ecosystem.”
Several companies have launched from the research hubs in Dallas-Fort Worth, such as Ampcare, which recently received FDA certification for its work in therapeutic neuromuscular electrical stimulation technology to help patients swallow. Allied Bioscience made waves by developing a product that kills the COVID-19 virus for up to three months on surfaces, which can be especially helpful for spaces that are difficult to clean in between use, such as school desks and airline seats.

Product development also is strong in Fort Worth, which last year launched the iter8 Innovation Community, a medical innovation district in the heart of the city. The new live-work-play district is meant to connect entrepreneurs to the healthcare and biotech industries that already exist there.
Many of the region’s largest healthcare employers are committing time and space to innovation, including Blue Cross Blue Shield’s C3 Innovation Lab in the West End District in downtown Dallas and Baylor Scott & White’s The Hive, which has worked to develop and improve the system’s top-rated MyBSWHealth app. Along Stemmons Freeway between the Medical District and Design District, J. Small Investments is collaborating with Lyda Hill Philanthropies to redevelop Pegasus Park, an expansive mixed-use project meant to boost local biotech initiatives. The 23-acre, 750,000 square-foot campus will include a 37,000 square-foot hub dedicated to life sciences innovation.
Hospitals and Health Systems
Several of the state and nation’s largest hospitals and health systems are based in Dallas-Fort Worth, even if not all of them have a large hospital presence in the area. Texas Health Resources has 29 hospitals in North Texas and a partnership with UT Southwestern. This gives THR’s community hospitals access to the expertise of the academic center while expanding UT Southwestern’s reach and influence in the region.
Baylor Scott & White Health has 50 hospitals across the state and is Texas’ largest nonprofit system. In 2018, BSW nearly merged with Houston’s Memorial Hermann, which would have created one of the country’s largest nonprofit systems, but the two parties amicably backed out of the agreement last year.
The COVID-19 pandemic has led to unprecedented coordination between local health systems, as competitors have come together to help deal with the crisis. “While this pandemic is unprecedented, our hospital systems have learned much over the past few months.,” said DFW Hospital Council President Steve Love. “Coordinated efforts have allowed us to nimbly respond to this fluid situation. As leaders, we attest to and applaud the unwavering efforts of our workforce in caring for those with COVID-19 and those seeking care for other urgent medical needs.”
The region is also home to several hospital systems that don’t have major hospital facilities here. Tenet Healthcare Corp., which recently moved from downtown Dallas to a new headquarters in Farmers Branch, is a Fortune 500 company with more than 113,000 employees, 65 acute care and specialty hospitals, and 490 outpatient locations stretching from California to Florida. Christus Health is based in Irving, but most of its 60 hospitals are in East and South Texas, with other facilities in New Mexico and Mexico. Steward Health also is based in Dallas, having moved its headquarters here from Boston in 2018. It has 35 community hospitals in nine states and Malta, making it the largest private, for-profit hospital operator in the country.
Education and Research
The impact of healthcare in North Texas owes a great deal to the numerous academic institutions that help supply the region with innovation, research, practitioners, and support professionals. Texas Christian University and The University of North Texas Health Science Center partnered to form North Texas’ newest medical school. The TCU and UNTHSC School of Medicine is taking a unique approach to medical education, focusing on integrating classroom learning with the clinical space, building up a corps of primary care physicians to help with the impending physician shortage, and developing empathetic graduates. UT Arlington is one of the nation’s largest producers of nursing graduates, with nearly 25,000 enrollees in the School of Nursing and Innovation in 2018. UT Dallas has created a pipeline of graduates to help run the healthcare industry’s business side, with both bachelor’s and master’s degrees in healthcare management. In Fort Worth, the Texas College of Osteopathic Medicine at UNT’s Health Science Center graduates the second most primary care physicians in the country.
The education and research anchor of the region is UT Southwestern Medical School, which has graduated 11,500 physicians since its founding in 1943 and brings in $469.5 million in research funding each year. The faculty includes four Nobel Prize winners in physiology, medicine, and chemistry. UTSW also hosts an “Innovation Tank” program, where physicians present ideas to improve care as they compete for $10,000 and institutional support.
Manufacturing
DFW is home to numerous manufacturers that supply the healthcare industry with the products they need. They include Kimberly-Clark, an $18.5 billion Fortune 500 company that makes protective gowns, cleansers, and gloves. It’s also a consumer force; about 25 percent of the world’s population uses one of its products every day.
Prestige Ameritech, the largest domestic surgical mask manufacturer in the nation, is based in North Texas. When the state and the Texas Military Department partnered with Prestige in early April, the North Richland Hills company was partially staffed by Texas National Guard members to enable 24-hour production, making about two million masks per week. The company’s 220,000-square-foot manufacturing facility produces masks and other medical products, such as N95 respirators, medical face shields, goggles, and gowns, and automated machinery that produces the masks.
The Future of Health
In an industry steeped in tradition, the COVID-19 pandemic has catalyzed change. Several healthcare trends have emerged during the crisis; here are five that are shaping up to profoundly impact the way services are delivered.
Telehealth is here to stay
Technology issues, reimbursement rates, and physician reluctance kept the usage of telehealth low before the pandemic. Healthcare analytics firm FAIR Health reports that telehealth represented just 0.12 percent of insurance claims in 2018. But when elective procedures were suspended in Texas and across the nation during the pandemic, and patients began avoiding physician offices, doctors quickly transitioned to virtual patient visits. Federal regulation followed, allowing for telehealth visits to be billed like an in-person appointment. Today, nearly all physicians and healthcare systems offer a telemedicine option. Market research company Arizton estimates telemedicine will become a $10 billion industry by the end of the year, with double-digit year-over-year growth of around 80 percent.Prospective Payments and Care Incentives
Due to a health insurance system that pays most physicians for the services they perform rather than maintaining the overall health of the patient, revenues collapsed when elective procedures were canceled during the pandemic. Fee-for-service payment also offers incentives to perform unnecessary care, as more procedures mean more revenue. Even before the pandemic, some physicians had been transitioning to value-based care with prospective payments, where providers are paid upfront per patient to keep the patient healthy. The pandemic only increased the calls to transition to this new model of compensation. “At the end of the day, employers are looking for more control of their annual spend with more predictable costs year over year,” says Scott Flannery, who oversees operations for United Healthcare in North Texas and Oklahoma. The prospective payment model can provide that consistency.
Fighting COVID-19 with an Old School Treatment
The Covid-19 pandemic has forced the medical industry to turn back to previously used techniques. Convalescent plasma has been a treatment since the 1918 flu pandemic, when plasma from the blood of recovered patients was used to treat those still suffering. At UT Southwestern, patients who have tested positive and then negative can donate their plasma and the antibodies it contains. Studies are underway to measure its effectiveness against the virus. A study in the Journal of the American Medical Association says that treatment in the early stages of the disease may be beneficial, but that more studies are needed.
Ongoing Consolidations
The healthcare market has been transitioning from independent hospitals, clinics, and doctor offices toward a model that brings everything together. Private practices are being snapped up by large health systems, corporations, and private equity firms. Becoming part of a larger business frees up physicians to focus on patients and no longer worry about running the company’s back office, dealing with real estate decisions, marketing, and other operations. But when a clinic becomes part of a system, the physicians lose control of other aspects. When the clinic is aligned with a hospital system, for example, costs tend to go up, as the physician may be incented to refer patients to the parent health system, even if that hospital is not the best or most cost-effective choice.
Addressing the Social Determinants of Health
Healthcare costs are rising unsustainably in the United States, accounting for 20 percent of GDP in recent years. But this hasn’t led to better results; outcomes are worse in the U.S. than they are in other countries that spend less on healthcare. Part of that inefficiency is the disparity in social determinants of health, such as education, transportation, healthy food options, and employment opportunities. Addressing these upstream needs can reduce spending on the back end and keep more people out of the hospital. This is leading to mental health professionals responding to 911 calls, checking in on the vulnerable, and other proactive measures.
Healthcare Roundtable
For North Texas community hospital executives, dealing with the coronavirus pandemic has highlighted the importance of strong leadership, communication, and collaboration.
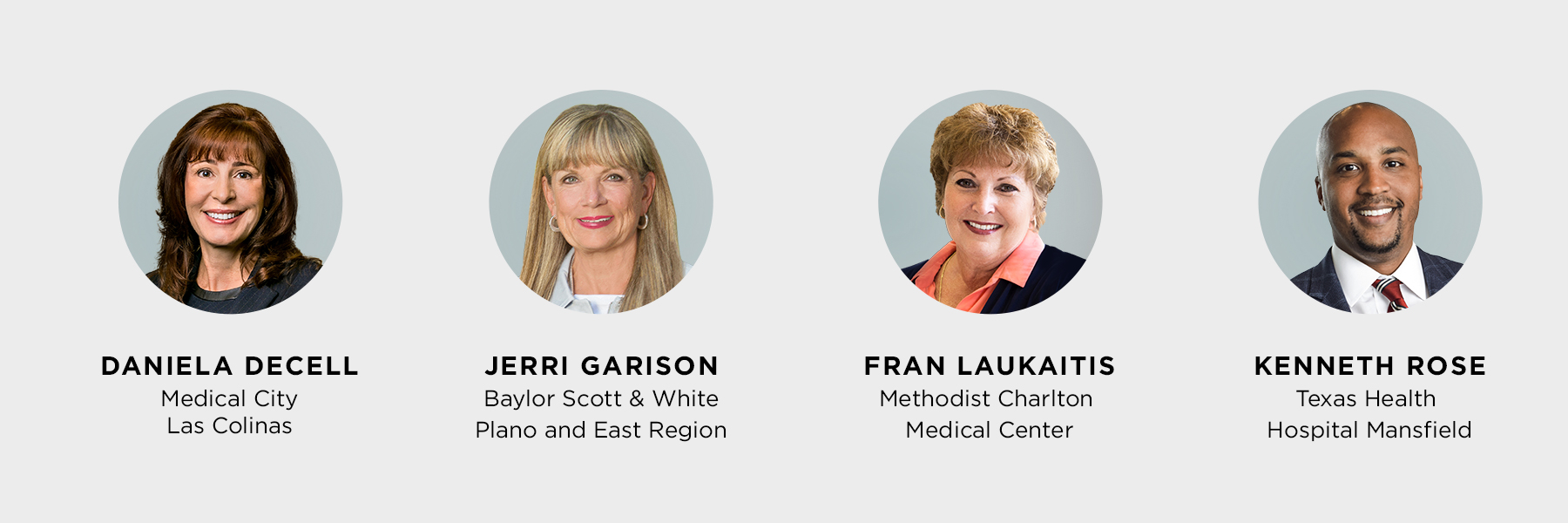
Flagship hospitals and corporate administrators usually get the headlines in healthcare coverage, but community hospitals are the institutions on the front lines of the industry. Embedded in the communities they serve, they play important roles in education, outreach, treatment, and employment opportunities for local residents. During the COVID-19 pandemic, these hospitals have been the primary points of contact for many who are experiencing symptoms. The facilities are tasked with making quick and safe decisions for their patients and staff—often with fewer resources and less fanfare than the flagship hospitals of the large health systems. Procuring effective personal protective equipment, transforming patient flow through the hospital, and dealing with unprecedented drops in revenue are just a few of the hurdles these leaders have to face—all while fighting a highly infectious disease. We recently invited four community hospital leaders from throughout the region—southern Dallas, Las Colinas, Mansfield, and Plano—to share their on-the-ground insights with us.
What is the most significant change on the way for healthcare delivery at acute care hospitals?
KENNETH ROSE: “It’s one that we have been engaged in for some time now, lowering and clarifying the cost. We have been somewhat insulated from price transparency as an industry in the past, but now in the consumer-based world, people expect to know and understand their healthcare costs. This journey will require us to lower the cost of healthcare.”
JERRI GARISON: “The use of technology has revolutionized our industry. We now have the ability to keep people out of the hospital longer by using televisits to assess conditions, using wearable technology to monitor chronic conditions at home, and using our electronic medical record across the continuum to remind our patients and members to get their regular screenings and see their doctors on a regular basis. These advancements put healthcare in the hands of the consumer, and that’s empowering.”
DANIELLA DECELL: “Learning to co-exist with COVID-19 while continuing to care for patients with other illnesses and emergencies may result in lasting changes for the healthcare industry. Masks and other personal protective equipment, for both patients and caregivers, coupled with technology that enables social distancing, may be common and best practice in the future.”
FRAN LAUKAITIS: “Technology—no question about it. This pandemic has accelerated a host of changes that will be with us in healthcare long after the virus is gone. I think the most significant change is the rapid expansion of telemedicine—more physicians seeing more patients virtually. For our hospitalized patients, virtual options have been a way to keep in touch with their loved ones as we have had to limit visitors. This technology has been nothing short of a lifeline for our patients, allowing them to communicate with their families.”
What do most business leaders not understand (or would find most surprising) about running a hospital?
LAUKAITIS: “Healthcare is a business, but our business is people. I think leaders in other industries may look at some of the decisions we make and think that may not be the smartest move financially. But in healthcare, it’s a balance, and our focus remains on our patients.”
ROSE: “How important people and culture are to our success. I think that everyone inherently knows that about business, but in highly regulated industries like healthcare, people may think that the legal and regulatory aspect is most important because it can shut you down. While that is important, there is no way to deliver safe and excellent healthcare to patients without hiring, engaging, and retaining great people throughout the organization.”
DECELL: “Unlike businesses that make or deliver a single product or service, hospitals provide many products and services and require a variety of businesses and experts to support the mission. Hospitals are an amalgamation of patients (consumers/clients) working with entrepreneurs (physicians) and a diverse group of skilled, talented employees (hospital staff) to obtain their desired or necessary service. Hospitals often house many small businesses under one roof—retail, marketing, entrepreneurs, restaurants, customer service, and others that are all focused on the patient.”
GARISON: “It may be counterintuitive, but we want to keep people out of the hospital—whether that’s being proactive and giving them tools they need to stay healthy or finding ways to deliver care that’s more convenient and cost-effective. There will always be a need for hospitals like ours, and we will always be here to deliver safe, high-quality care; but we also realize that we play an important role in empowering consumers and enabling them to play a more active role in their health.”
What has been the best part of leading your hospital?
GARISON: “The best part of leading in these unprecedented times is the teamwork I have observed within our hospital and throughout our community. We have been overwhelmed by the support in the form of inspirational messages, parades, food for our employees, masks, and recognition of our healthcare heroes. … It’s inspiring to be part of a community with a strong desire to make a difference.”
“There’s still so much we don’t know about how this virus will evolve, and I think that kind of uncertainty is challenging for any leader.”
Fran Laukaitis, Methodist Charlton Medical Center
LAUKAITIS: “We are meeting our mission at a time when our patients across southern Dallas need us the most. COVID-19 has had a significant impact on our communities, and it’s more important than ever that our patients know we are here for them. It’s a pleasure and a privilege to lead the team at Methodist Charlton. They are all so supportive and positive, even during times of uncertainty.”
ROSE: “The best part has been seeing how our new hospital project has continued to progress and develop, even through challenging times.”
DECELL: “The best part of leading during this unprecedented time has been the amazing attitude and teamwork of the staff. Our colleagues truly embody a ‘you first’ mindset and have shown boundless compassion for COVID-19 patients and their families. Each time a COVID patient is discharged, our caregivers celebrate as if it were their own family member. A close second has been experiencing the incredible outpouring of love and support from the community. From ‘park and pray’ events to hand-drawn signs of support and meal donations, we have been richly blessed by the citizens of Irving and surrounding communities.”
And what has been the most challenging?
ROSE: “The most challenging aspect is how to focus on developing a new hospital from scratch while learning about how to operate in a COVID-19 world. This exercise is forcing us to think differently about how we will deliver care when we open in December.”
DECELL: “One big challenge has been the significant swing in patient volume. We experienced an initial COVID-19 surge in March, then a rapid decline in volume as elective surgeries were postponed, and some patients delayed vital medical care, followed by the current resurgence of COVID-19 cases again.”
GARISON: “The evolving nature of the pandemic. With less than 200 days of experience with COVID-19, our clinical teams continue engaging in ongoing discussions with public health officials to gather the latest information and update our clinical protocols accordingly. We have been blessed within our system that of our patient-facing employees who had an exposure to a COVID-positive patient, less than 1 percent were found to be positive. Over time, as our collective knowledge has increased, including guidance from the Centers for Disease Control, our protocols have changed, and these positives are much less frequent.”
LAUKAITIS: “The most challenging part of leading any hospital right now is the uncertainty of this virus and what the future may hold. We have never seen a virus like this one. We have never dealt with anything quite like it. There’s still so much we don’t know about how this virus will evolve, and I think that kind of uncertainty is challenging for any leader.”
At what point did you realize that healthcare administration was the career for you?
GARISON: “I started my career as a nurse. As I progressed in my career and transitioned to administration, I knew that the ability to speak as a clinician would help me advocate for the bedside caregiver. This advocacy for our team is what I have been passionate about my entire career, and I hope that I have been able to make a difference.”
ROSE: “During a summer internship at what was then Florida Hospital Orlando (now AdventHealth Orlando), I worked in its mission development department. I was so struck by the opportunity in healthcare to minister to people through our work. That made this career a perfect fit for me.”
LAUKAITIS: “I have been in healthcare for 45 years, and I’ve had a lot of great mentors along the way. I spent decades as a bedside nurse. For me, being a hospital president is just another way to serve patients.”
DECELL: “I had meningitis in my late teens and spent two weeks in a hospital intensive care unit. The compassion of the nurses in the ICU made a lasting impact on me; they contributed to my healing in ways I could not have imagined. I decided to become a nurse myself. For 12 years, I worked as a critical care nurse, caring for the sickest of patients. I had exceptional mentors who encouraged me to use my nursing and leadership skills to help improve the lives of patients and colleagues in the hospital in an administrative role.”
What is top of mind for you right now in leading your hospital?
LAUKAITIS: “The safety of our patients and everyone who works here. There’s so much uncertainty when it comes to this virus, so safety will remain our focus. But also, reassurance is important. Part of my job is to reassure the staff that we are doing everything within our power to keep them safe.”
ROSE: “My current top priority is building and maintaining a strong culture. As a new team building a new hospital, we are getting a once-in-a-lifetime opportunity to form a team culture from scratch, and I will not waste that opportunity.”
DECELL: “I am focused on supporting our hospital and medical colleagues as we tackle this new surge of COVID-19 cases in North Texas. In addition, I want to continue to educate and remind the public that they play a vital role in saving lives—social distancing, hand sanitizing, and masks work.”
GARISON: “My top priority is making sure we have a safe environment for our employees and our patients who must feel comfortable getting the care they need. Delaying care has been a critical issue; estimates of those who are currently putting off care top 50 percent. That’s particularly worrisome in those patients who have chronic conditions or emergent issues.”
How have you collaborated with other leaders during the COVID-19 pandemic?
DECELL: “The first thing that comes to mind is the saying, ‘It takes a village.’ It was understood from the start that navigating the pandemic would require strong, coordinated leadership and communication. Our objectives were to protect our colleagues, both financially and personally, and to protect our facilities so we can continue to provide safe, high-quality care to our communities.”
GARISON: “This is a time of uncertainty, but the North Texas community has approached the challenges we’ve faced with a strong spirit of collaboration. We have worked in close collaboration with our elected officials and the North Central Texas Trauma Regional Advisory Council to share data, education, and resources. We are also working closely with the business community by providing guidance on prevention and testing.”
LAUKAITIS: “The leaders at the individual Methodist hospitals have spent a lot of time collaborating at the system level. Consistency in execution and in messaging is incredibly important at a time like this. We have worked hard to make sure we are all on the same page.”
ROSE: “Our corporate parents have been very supportive and encouraging of bringing hospital leaders together. I have been leaning heavily on their guidance [and communication] and COVID policies. We have frequent calls with corporate and local hospital leadership in various markets throughout our company. Collaborating and learning new things every day about processes proves to be valuable.”






