UT Southwestern is on the leading edge of a surgical technique that treats prostate cancer without some of the impactful side effects. It features an MRI-guided device that uses ultrasound heat to destroy the tumors, and no academic medical center has performed more of them than UTSW.
The American Cancer Society found that more than 250,000 new prostate cancer were detected in 2022, and 34,500 people died from prostate cancer last year. One in eight men will eventually be diagnosed with prostate cancer which usually develops in older men. Prostate cancer is the second leading cause of cancer death in American men, behind lung cancer. One in 41 men will die from it. Even though the deaths and impact of prostate cancer are nearly as significant as breast cancer, the amount of research and funding for its treatment is far below that of breast cancer.
Conventional treatment involves a combination of surgery and radiation to remove the tumor. But these treatments leave a lot to be desired in terms of treating the disease and preserving the quality of life, says Dr. Daniel Costa, an associate professor of radiology at UT Southwestern Medical Center who was involved in the trials of this technology and performs the surgery. He says that when men are diagnosed with prostate cancer, patients can sometimes push back because of the side effects, namely sexual impotence and incontinence.
Surgery and radiation often damage other tissue and organs near the prostate. Because prostate cancer often needs to be treated multiple times, some men would rather risk leaving cancer for longer to maintain their hygiene and sex lives. But ultrasound technology solves both those problems.
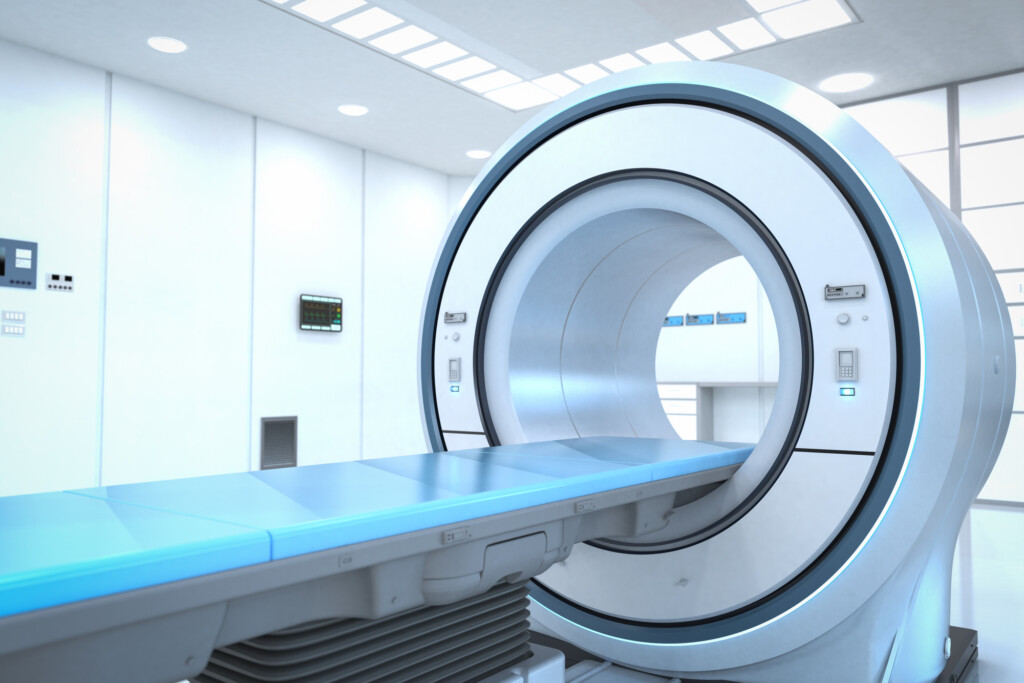
Called TULSA, which stands for Transurethral Ultrasound Ablation, the minimally invasive surgery is done by inserting a device guided by MRI imaging through the urethra and delivering precise amounts of ultrasound to affected areas in the prostate while using the MRI images to spare healthy tissue nearby. Unlike surgery and radiation, the side effects are minimal, and if the cancer returns, those treatments are still options.
The urologist places the probe, and the radiologist executes the treatment. The device causes the tissue to vibrate and increase the temperature. The MRI allows the physicians to preserve the nerves connected to sexual performance and incontinence, which can be difficult to locate during surgery. The probe rotates to find the tumor during the procedure, which usually lasts less than an hour.
Costa and UTSW were part of the trial for the device, which was developed in Canada after a company spun off from the University of Toronto. That trial led to FDA approval, and Costa began treating patients with it in 2020. Late last year, the medical center successfully treated its 100th patient with TULSA, more than any academic medical center.
“This is not about me. It’s about the treatment and hopefully what I can do to patients in our community,” Costa demurs. “But It is legitimate to say that we were pioneers. Nobody used this before we did in the great majority of the United States.”
Medical professionals often work in silos without collaboration between subspecialties, but Costa says that radiology and urology have to partner closely to make this treatment happen. Urologists work with the patients to identify suitable candidates for TULSA while radiologists perform the operation and pass the patient back to the urologist for follow-up care.
“There is not much cross-fertilization in medicine, and physicians tend to see physicians from another specialty as a threat, or somebody who is taking their patients,” Costa says. “We are very fortunate to have built a partnership over decades here that allows us to work while truly keeping the patient’s best interests in mind. There is not as much territoriality.”
Looking forward, this technology may have other applications. Costa says the technology is being tested to treat uterine fibroids, which are non-cancerous growths on the uterus that develop during childbearing years and can cause pain, excessive bleeding, constipation, or excessive urination. Other work is looking at using focused ultrasound to treat bone cancer and in the brain to treat tremors and Parkinson’s disease.
Finding a treatment that is both more effective and has fewer side effects is a physician’s dream, and Costa is proud of the physicians at UTSW for being a part of this research and treatment.
“There has been a need for quite a while for better treatments in terms of being less invasive with fewer side effects to make it so that the solution to the problem is not more burdensome than the problem itself,” Costa says. UTSW physicians are on the leading edge of doing just that.
Get the D CEO Healthcare Newsletter
Author