A public-relations executive in her mid-thirties representing a large, modern physician practice shook her head in puzzlement.
Her physician client liked to talk about how his practice was not “a Marcus Welby shop,” meaning that its approach and technology reflected the best the 21st century had to offer. As she walked a visitor toward the office-building exit, she confided, “He keeps talking about this Marcus Welby. I think it’s someone he went to business school with.”
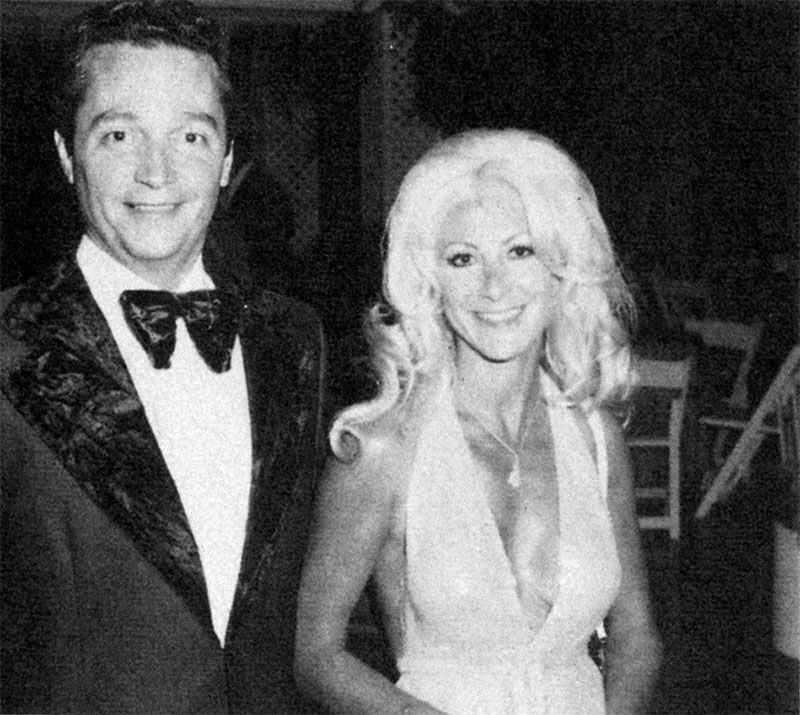
Marcus Welby, the iconic primary care physician who treated patients with inexhaustible kindness and compassion, was at or near the top of the television network ratings and a staple of ABC’s lineup from 1969 to 1976. Marcus Welby, M.D., rose to No. 1 in the Nielsen ratings in its second season, viewed regularly in about 1 out of 4 American homes. Stars Robert Young (Welby) and James Brolin, who played partner Steven Kiley, won Emmy Awards in 1971, and Young won a Golden Globe in 1972.
Predictably, most diseases could be cured within the show’s hour-long time slot. If not, Welby would at least ease the patient’s emotional burden. Young received thousands of letters from fans asking for advice on medical or personal problems.
There was some debate at the time about whether Welby’s image was good for U.S. physicians. Welby could not have been a more positive face for American medicine. However, some doctors were concerned that his tireless customer service and patient bedside manner would lead to unrealistic expectations from patients. Some even believed that Welby contributed to the rise in malpractice lawsuits.
Dr. Don McCanne, a senior health policy fellow at Physicians for a National Health Program, wrote a 2011 blog post titled, “How would Marcus Welby, M.D., fare in an ACO?”
The broader question is whether Welby would be able to function effectively under today’s government regulation and insurance bureaucracy. Welby and Kiley had one nurse/receptionist. It is no wonder that they could spend so much time with the patients. The pair comprised the ultimate patient-centered medical home—no need for National Committee for Quality Assurance certification.
During the show’s run in the late 1960s and early 1970s, physician payment from Medicare was based on a system of customary, prevailing, and reasonable charges. From the mid-1970s through the mid-1980s, government implemented a series of cost controls. Nearly half of all medical bills were paid out of pocket by commercially insured patients, compared with less than 10 percent today.
The appeal of primary care as a career seemed endless at the time. During the show’s final season in 1976, a Department of Health, Education and Welfare advisory committee predicted a surplus of 145,000 primary-care physicians by 2000.
It did not work out that way. In a 2005 survey of U.S. med school seniors, half considered limits on income and lifestyle as serious obstacles to entering a primary care practice. However, the No. 1 deterrent, respondents said, was the lack of positive role models or mentors. There were no more Marcus Welbys. Instead, about 3 out of 4 physicians between age 50 and 65 said medicine was increasingly unsatisfying, according to a 2004 survey.
Physician recruiter Merritt Hawkins CEO Mark Smith testified before a U.S. House subcommittee in July 2012 on the decline of solo physician practices.
“Virtually no one wants to be Marcus Welby anymore,” Smith said.
He said small physician practices face five major barriers: flat or declining reimbursement; increasing regulatory and administrative paperwork; increasing malpractice insurance costs; health information-technology mandates; and the effects of health-delivery reform. A 2011 survey of final-year medical residents found that only 1 percent wanted to work as solo practitioners like Welby. Only 2 percent of Merritt Hawkins job searches involved recruitment of solo practitioners in 2011, down from 17 percent five years previously.
Said Phillip Miller, Merritt Hawkins vice president of communications, of solo practitioners: “No one is looking for one. No one wants to be one.”
In 1973, only 15 percent of physicians voiced regret about their career choice—and Welby certainly embodied that sense of certainty. By 2002, more than half of physicians over 50 years old said they would not choose medicine as a career again.
Welby always seemed suspicious of specialists, so it is questionable how skilled he would have been at care coordination. However, even he moved his practice to a hospital toward the end of the show’s run.
Baby boomer physicians often deride the fact that newly minted doctors want lives that are more balanced. Many older physicians still work Welby-style 70-to-80-hour weeks. White men dominated the profession in the 1970s. Fewer than 8 percent of physicians were women. Women now make up about half of incoming medical school classes. Research shows that they work fewer hours, largely because of family obligations.
“The older ones are being pushed out (of the system). Many are pissed off and leaving. They have a different view of medicine than the new ones. Being a doctor defined who they were,” said Ripley Hollister, Colorado family physician and Physicians Foundation board member. “It was their purpose in life. Younger doctors work maybe 40 hours a week. They see it more as employment than a profession. They have a different view about quality of life. They won’t be quite the workforce (in quantity of hours).”
Darrell Kirch, president of the Association of American Medical Colleges, believes that new physicians have a more expansive view of medicine and life, and considers that a positive development.
“I see no evidence that indicates that their ethical commitment is any weaker, that they care any less for patients,” he told the Associated Press.
In some ways, Welby was the predecessor of a concierge physician. He was available 24/7 and would spend as much time as the patient needed. Welby, of course, did not get a monthly retainer fee. In fact, he was quick to provide uncompensated care.
The spirit of Marcus Welby lives in today’s physicians. However, his business model is swiftly disappearing from the American landscape. Welby’s practice style could not survive financially in today’s medical culture: having to see one patient every 15 minutes to keep the practice open; seeking insurance preauthorization for treatment; and being office-bound.
New Hampshire physician and Dartmouth Medical School professor Robert Wortmann wrote:
“It’s a bit unfair to consider Generation X physicians to be unprofessional. Times change and so does our profession. Marcus Welby did not have a working wife, a computer, a preauthorization clerk in his office, or a utilization review committee in his hospital.
When he started practice, there were only two non-steroidal anti-inflammatory drugs available, and hypertension was not treated until it became symptomatic. Few hospitals had coronary-care units. Compared with today’s environment, he had so few tools to work with that his most valuable patient care resource was his time.”
The circumstances under which America’s physicians will do their jobs will change more in the next decade than they have in the past 50 years. The Physicians Foundation, based in Boston, has identified some of the most pressing issues facing U.S. doctors—the uncertainty over the Affordable Care Act, where the nation will find the capacity to treat millions of newly insured patients, the continuously expanding administrative burden, the industry’s relentless consolidation to gain market leverage and the forces nibbling away at practice autonomy.
In his new book So Long, Marcus Welby, M.D.: How Today’s Health Care Is Suffocating Independent Physicians—and How Some Changed to Thrive, D Healthcare Daily founding editor Steve Jacob draws on dozens of interviews and more than 500 published sources to cover these issues and describe how the landscape is changing for doctors.