Hockey
What We Saw, What It Felt Like: Stars-Golden Knights, Game 2
It’s time to start worrying.
By Sean Shapiro and David Castillo
Trending
1
Business
Executive Book Club: Recommended Reading From North Texas C-Suiters
By D CEO editorial team
Guides

Restaurants & Bars
Where to Find the Best Italian Food in Dallas
From the Tuscan countryside to New York-inspired red sauce joints, we recommend the best of every variety of Italian food available in North Texas.
Advertisement
50 Greatest Stories
View All
Sex & Drugs
Lords of an Underground Empire
Biography & Memoir
You Can Go Home Again
History
Akin vs. Dahl

High Society
Why Hockaday Girls Are Different
Romance
The Stoneleigh, Heartbreak Hotel

Fascinating People
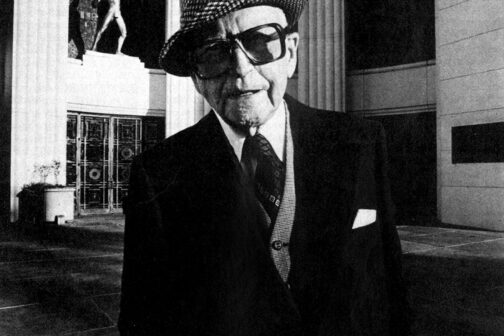
A Legend in His Own Mind
Sex & Drugs
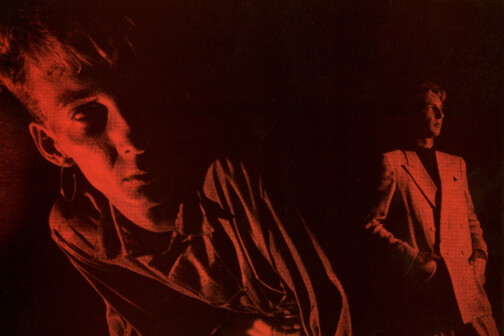
Ecstasy & Agony at the Starck Club
True Crime
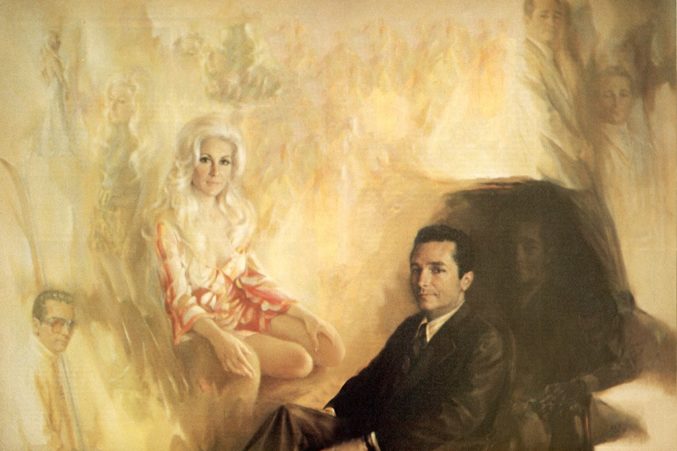
Is Priscilla Davis’ Story True?
Fascinating People
Max Goldblatt’s Last Hurrah
Our Magazines
Enjoy unlimited access to all of our incredible journalism, no matter how you prefer to read.
Hot Properties
View All
Hot Properties
Hot Property: An Architectural Gem You’ve Probably Driven By But Didn’t Know Was There
It’s hidden in plain sight.
By Jessica Otte
Advertisement
News
View More
Local News
Mayor Eric Johnson’s Revisionist History
In February, several of the Mayor’s colleagues cited the fractured relationship between Broadnax and Johnson as a reason for asking the city Manager to resign. The mayor says those relationship troubles were “overblown” by the media.
Food & Drink
View More
Restaurant Reviews
You Need to Try the Sunday Brunch at Petra and the Beast
Expect savory buns, super-tender fried chicken, slabs of smoked pork, and light cocktails at the acclaimed restaurant’s new Sunday brunch service.
Advertisement
Arts & Entertainment
View More
Arts & Entertainment
DIFF Preview: How the Death of Its Subject Caused a Dallas Documentary to Shift Gears
Michael Rowley’s Racing Mister Fahrenheit, about the late Dallas businessman Bobby Haas, will premiere during the eight-day Dallas International Film Festival.
By Todd Jorgenson
Advertisement
Sports
View More
Hockey
What We Saw, What It Felt Like: Stars-Golden Knights, Game 2
It’s time to start worrying.
By Sean Shapiro and David Castillo
Advertisement
Home & Garden
View More
Home & Garden
Past in Present—A Professional Organizer Shows You How To Let Go
A guide to taming emotional clutter.
By Jessica Otte
Advertisement
Living
View More
Publications
Botanical Mix Updates New Downtown Storefront for Spring
Florist Shane Friesenhahn gives a colorful refresh to his shop near Pacific Plaza Park.
By Kathy Wise
Advertisement
Business
View More
Commercial Real Estate
What’s Behind DFW’s Outpatient Building Squeeze?
High costs and high demand have tenants looking in increasingly creative places.
By Will Maddox
Latest

Local News
Mayor Eric Johnson’s Revisionist History
In February, several of the Mayor’s colleagues cited the fractured relationship between Broadnax and Johnson as a reason for asking the city Manager to resign. The mayor says those relationship troubles were “overblown” by the media.

Media
Will Evans Is Now Legit
The founder of Deep Vellum gets his flowers in the New York Times. But can I quibble?
By Tim Rogers

Restaurant Reviews
You Need to Try the Sunday Brunch at Petra and the Beast
Expect savory buns, super-tender fried chicken, slabs of smoked pork, and light cocktails at the acclaimed restaurant’s new Sunday brunch service.
Get our weekly recap
Brings new meaning to the phrase Sunday Funday. No spam, ever.

Arts & Entertainment
DIFF Preview: How the Death of Its Subject Caused a Dallas Documentary to Shift Gears
Michael Rowley’s Racing Mister Fahrenheit, about the late Dallas businessman Bobby Haas, will premiere during the eight-day Dallas International Film Festival.
By Todd Jorgenson

Commercial Real Estate
What’s Behind DFW’s Outpatient Building Squeeze?
High costs and high demand have tenants looking in increasingly creative places.
By Will Maddox
Advertisement
Latest

Hockey
What We Saw, What It Felt Like: Stars-Golden Knights, Game 2
It’s time to start worrying.
By Sean Shapiro and David Castillo

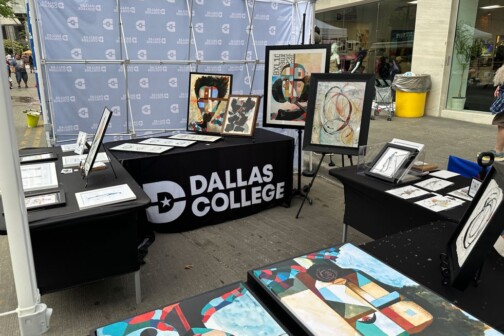
Business
Executive Education Guide
During times of economic disruption, professionals and executives turn to higher education so they can make a strategic career move. Fortunately, Dallas-Fort Worth has several advanced degree programs recognized throughout the country for excellence and results.
Get our weekly recap
Brings new meaning to the phrase Sunday Funday. No spam, ever.
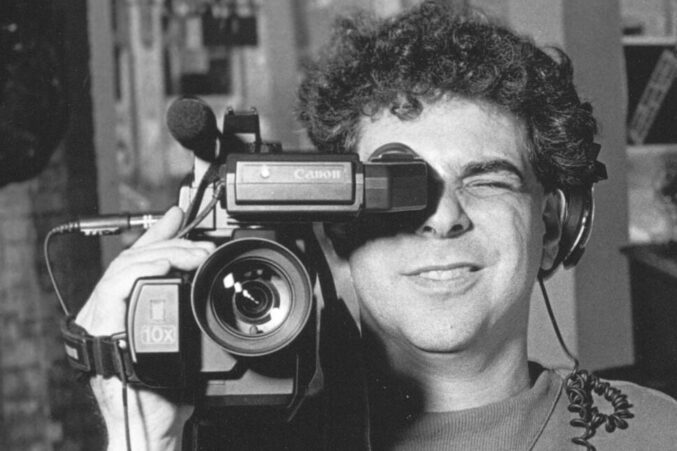
Arts & Entertainment
VideoFest Lives Again Alongside Denton’s Thin Line Fest
Bart Weiss, VideoFest’s founder, has partnered with Thin Line Fest to host two screenings that keep the independent spirit of VideoFest alive.
By Austin Zook

Local News
Poll: Dallas Is Asking Voters for $1.25 Billion. How Do You Feel About It?
The city is asking voters to approve 10 bond propositions that will address a slate of 800 projects. We want to know what you think.